Diabetes mellitus is a systemic disease that, if not adequately controlled, can have a major impact on the quality of life of sufferers, not least because of the complications that can affect different body districts, first and foremost thevisual apparatusalong with the kidneys, peripheral nervous system and cardiovascular system.
The most important and frequent ocular complication of diabetes, both type 1 and type 2, is the Diabetic Retinopathy, which in some cases can be further aggravated by the onset of theDiabetic Macular Oedema, a pathological condition that can lead to severe damage to central vision.
Before giving you specific information on the two diseases, let us summarise the functions that the pharmacist can be called upon to perform.
The role of the pharmacist
There are many areas in which the pharmacist's intervention is prominent
– Self-diagnosis
– Therapeutic adherence
– Adherence to monitoring protocols
Self-diagnosis
I self-diagnosis test consist of a series of first-instance analytical services, which can be carried out directly by patients, as a self-check, at home or alternatively can be used with the support of a health professional, at public and private territorial pharmacies.
Self-diagnosis tests include the blood glucose control, which is often administered during screening campaigns organised in the territory.
Since the metabolic control of diabetic disease also involves the prevention of hypertension, hypercholesterolaemia and obesity, other self-diagnosis tests such as the following are also important:
– Cholesterolaemia (total and fraction)
– Triglyceridemia
– Real-time measurement of haemoglobin and glycated haemoglobin.
All these services are part of the activities that pharmacists will be called upon to perform in the Service pharmacy which this year seems to be moving towards fuller implementation: first in the nine pilot regions, to be joined by the entire country in 2021-22.
Therapeutic adherence
The pharmacist can perform a counselling function in stimulating the diabetic patient to:
- fully comply with prescriptions, both with regard to the drugs to be taken and the methods of taking them indicated by the doctor.
- adopting a healthy lifestyle, following a balanced diet and moderate physical activity to control overweight, counteracting sedentary lifestyles.
Adherence to monitoring protocols
The diabetic patient, if he wants to stay healthy and prevent complications, must undergo systematic medical check-ups.
The pharmacist can play an important informative role in encouraging the patient to have regular check-ups, firstly with the family doctor and/or diabetologist, and when necessary more specific examinations by specialists such as the cardiologist, ophthalmologist and nephrologist.
Retinopathy and diabetic macular oedema
Pathophysiology and classification
The pathogenesis of Diabetic Retinopathy (DR) and especially Diabetic Macular Oedema (DME) is multifactorial. There is a growing consensus in scientific circles that it is more of a neurovascular pathologythan of a pure microangiopathy; in fact, in addition to damage to the vascular network, severe and early structural and functional alterations of the retinal neuronal cells.

The main pathways activated by hyperglycaemia and implicated in the development of DR are: stimulation of the polyol pathway (sorbitol-aldose reductase pathway), the diacylglycerol (DAG) pathway, activation of the inflammatory and leucostasis cascade, and increased production of advanced glycosylation end-products (AGEs). These processes increase the basal level of oxidative stress, causing a dysfunction and finally apoptosis of retinal neuronal cells. Increased oxidative stress also causes endothelial damageleading to an alteration in blood flow regulation mechanisms, a reduction in capillary perfusion and a breakdown of the inner blood-retinal barrier (BER), with increased permeability. Clinically, this results on the one hand in peripheral capillary obliteration, and on the other hand in macular hyperpermeability, resulting in EMD. Escalating tissue damage leads to a clinical progression of DR, from milder formscharacterised by venous abnormalities (duplications, irregularities? of vascular calibre), microaneurysms and IRMAs (Intra-Retinal Microvascular Abnormalities), to those more advanced.
Internationally, it is traditionally accepted to classify DR into:
– non-proliferating form (NPDR), characterised by microaneurysms, altered retinal capillary perfusion, multiple cottony exudates, flame haemorrhages, and IRMA.
– proliferating form (PDR)characterised by the occurrence of epiretinal neovascularisation or on the optic nerve head. When haemovascularisation occurs, due to bleeding of the newly formed abnormal vessels, or when the neovascularisations occupy a large portion of the optic papilla, even in the absence of haemovascularisation, we speak of high-risk PDR.
Risk factors
Risk factors for the development of DR can be classified into modifiable and non-modifiable. Those predisposing to EMD are the subject of greater controversy, but can be considered substantially overlapping with those associated with DR.
Not modifiable
- Duration of diabetes
- Pregnancy
- Puberty
- Genetic predisposition
Modifiable
- Hyperglycaemia
- Arterial hypertension
- Dyslipidaemia
- Obesity and metabolic hormones
- Systemic and local inflammation
- Oxidative stress
- Vitamin D levels
Among the parameters that cannot be changed, the duration of diabetes is undoubtedly the most important risk factor, as is clearly evident for type 1 diabetes: in young people with type 1 diabetes lasting less than 5 years and in prepubertal age, the prevalence of DR is negligible, whereas if diabetes is diagnosed after the age of 30, the prevalence of retinopathy is 20% after 5 years of disease, 40-50% after 10 years, and over 90% after 20 years. This relationship is not as clear in type 2 diabetes cohort studies, probably due to the competing risk of mortality in a generally older cohort of subjects with more co-morbidities.
The pregnancy constitutes a risk factor for the progression of RD and EMD, especially in patients with type 1 diabetes. Possible mechanisms behind this phenomenon include both hormonal and immune theories.
Turning to modifiable factors, there is a directly proportional relationship between the blood glucose level e frequency of retinopathy. In addition to the absolute value of blood glucose and HbA1c, short-term variability of these values, such as spikes in postprandial glucose or sudden hypoglycaemia, was also found to be associated with an increased risk of microvascular complications.
Tight glycaemic control is much more effective in preventing or delaying the onset of DR in patients with diabetes without retinopathy than limiting the severity of DR after its onset.
Current guidelines suggest maintaining an HbA1c value between 6.5 and 7.5%. According to a recently published Cochrane meta-analysis, however, there is no concrete evidence on any specific treatment goals, but rather a personalised approach is recommended, with treatment goals individualised according to age, disease progression, risk of hypoglycaemic episodes, and the patient's psychological factors.
Several epidemiological studies have identified thehypertension as a risk factor for both DR and EMD; in fact, tight blood pressure control (<150/85 mmHg) in patients with type 2 diabetes has been shown to reduce the risk of microvascular disease by 37%, the rate of DR progression by 34% and the risk of worsening visual acuity by 47%. In contrast to hyperglycaemic control, the protective effect of blood pressure control is quickly lost when intensive control is discontinued.
Recent familial aggregation studies have also demonstrated a hereditary tendency for severe retinopathy in individuals with both type 1 and type 2 diabetes, regardless of shared risk factors.
Diagnosis
Several imaging methods play a primary role in the diagnosis and management of the patient with DR, including colour retinography, retinal fluorangiorrhaphy, OCT, and angio-OCT.
The diagnostic gold standard still remains the stereographic colour retinography.
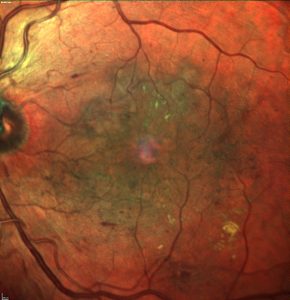
L'OCT is a method of great importance in the assessment of macular status in DR patients and also provides useful information on structures such as the vitreo-retinal interface, the thickness of the nerve fibre layer and ganglion cell layer, and the choroid.
In addition, OCT makes it possible to assess quantitative aspects and qualitative characteristics specific to theEMDallowing their clinical classification and the identification of the correct therapeutic approach.
Regardless of retinal thickness, EMD can be classified according to fluid site, and three different patterns have been proposed:
– cystoidcharacterised by intraretinal pseudocysts
– intraretinalcharacterised by tissue thickening without evidence of discrete cysts
– serous detachment of the neuroepitheliumas accumulation of fluid in the subretinal space
L'angio-OCT is a relatively recent method that non-invasively, rapidly, and three-dimensionally assesses retinal and choroidal vascular layers.
Screening
Current scientific evidence shows that the implementation of screening programmes and early intervention can dramatically reduce the proportion of blindness related to DR and EMD. Treatment efficacy is strongly correlated with adherence to treatment protocols suggested by international multicentre studies.
RD screening in ophthalmology can be performed by the following methods: ophthalmoscopy (direct and/or indirect), biomicroscopy (slit lamp with both contact and non-contact lenses) with dilated pupils; colour retinography with non-mydriatic fundus cameras. Digital retinography is a promising model for screening in the field and is a perfect example of telemedicine. This examination exploits digital recording of the image obtained without mydriasis, and allows remote transmission and reporting by qualified reference facilities. Recently, retinal imaging devices have been developed that aim to facilitate DR screening by implementing the technologies offered by telemedicine. These devices connect to the smartphone and acquire the retinal image like a fundus camera. These instruments are portable and easy to install, and can also assess the anterior segment. However, they require pupil dilation and are still limited in the perfect visualisation of the extreme retinal periphery.
A DR screening programme must be associated with timely referral to second- or third-level facilities ('referral system') that can offer appropriate ophthalmological care. Guidelines suggest that without appropriate access to ophthalmic care, the benefits associated with screening patients with DR are lost.
Le general recommendations for screening of DR, as indicated by national and international guidelines, are as follows:
- Patients with type 1 diabetes should have their dilated eye fundus assessed for the first time five years after diabetes diagnosis (or at puberty).
- Patients with type 2 diabetes should have an initial assessment of the dilated ocular fundus upon diagnosis of diabetes.
The frequency of checks must be:
- in the absence of retinopathy, at least every 2 years;
- in the presence of mild non-proliferative retinopathy every 12 months;
- in the presence of moderate non-proliferating retinopathy, every 6-12 months;
- in the presence of proliferating retinopathy, every month;
- in the presence of diabetic oedema not involving the macula, every 3 months;
- in the presence of diabetic oedema involving the macula, every month.
Pregnancy is a factor in the development or progression of DR and, therefore, diabetic women planning to have children should have a complete eye examination before and during gestation, with follow-up until delivery. Gestational diabetes is not a risk factor for DR.
CONCLUSIONS
Diabetic retinopathy represents one of the most serious complications of diabetes in individuals of working age. For proper management, and to reduce its social and economic burden, a strict programme of:
- primary prevention: control of risk factors, including glycaemia, high blood pressure, dyslipidaemia,
- secondary prevention with early detection of retinopathy.
- tertiary prevention (avoiding blindness in patients with DR).
Screening of the diabetic population by means of ophthalmoscopic/retinography examinations must have a widespread distribution throughout the territory; telematic dispatch to certified reading centres (telemedicine) is becoming increasingly important for this purpose.
This article can also be downloaded in PDF format Card No. 11 - The pharmacist and the ocular complications of diabetes
© Copyright 'l'Oculista italiano' - January 2020
Dr. Carmelo Chines
Direttore responsabile
