The Italian government took important decisions in the early months of 2020 that provide for a greater commitment to the fight against l'antibiotic resistancewhich will see Pharmacies at the forefront.
We devote this sheet to the new functions that the pharmacist will be called upon to perform in this context and to a brief description of the phenomenon of antibiotic resistance, with a particular focus on ophthalmology.
Awareness-raising and training campaigns
Accordingly, the Government will engage in actions to combat the phenomenon of antibiotic resistance, through:
- promoting informed consumption of antibiotics with awareness-raising campaigns in pharmacies
- good practices for hospital infection control
- the funding of research and continuing education of doctors, pharmacists and other health professionals involved.
In particular, the government has undertaken to put in place initiatives to provide for awareness and information campaigns for citizens on the subject of antimicrobial resistance promoted within the individual pharmacies belonging to the widespread network of public and private pharmacies affiliated with the national health service, defining appropriate measures in line with the 'service pharmacy' regulations.
In the area of training, the government will promote, with reference to its own competencies, the implementation of specific training courses for doctors, pharmacists and other healthcare professionals involved, focusing on resistance prevention strategies, so that they can acquire the most effective ways of raising awareness, including through health education campaigns, among patients on the safe use of antibiotics, with particular regard to correct intake, compliance with doses and schedules, and the dangers of storing any remaining stocks of the drug.
Antibiotic resistance in Ophthalmology
In recent decades, the inappropriate use of antibiotics (especially of molecules with a broad spectrum of action), the administration of sub-optimal dosages and the massive first-line use of molecules with a high capacity to generate resistance, have led to the emergence of the antibiotic resistance.
In recent years, in fact, antibiotics have been used massively, not only for therapies on humans, but also in livestock and animal husbandry and in food production, to the extent that they have led to the selection of microbial strains that have acquired multiple resistances, i.e. directed towards many (if not all) antibiotic families.
When people talk about antibiotic resistance and multi-resistant bacteria, the dreaded 'superbugs', they often think of new diseases and/or pandemics spreading out of control. In reality, the real threat is less obvious, but more insidious, as it lurks precisely in places of care, such as hospitals.
Among the main problems are the presence of fluoroquinolone-resistant strains and methicillin-resistant staphylococci (MRSA: Methicillin-Resistant Staphylococcus Aureus), which have recently been joined by bacterial strains resistant to all antibiotics (MDR: Multi-Drug Resistant).
The problem of resistance has long emerged in systemic therapies, but also specifically affects antibiotics for ophthalmic use.
Antibiotics and their correct use
With regard to the problem of antibiotic resistance, one must evaluate eye diseases by degree of importance: the main division must be made between the conjunctivitis and all other forms that can be considered serious or for which pharmacological intervention is certainly required, such as keratitis, endophthalmitis, dacryocystitis and phlegmon.
The ocular surface is actually not sterile, but is characterised by the presence of a microbiotawhose composition may vary depending on a variety of factors.
The most represented bacteria are the Staphylococcus epidermidis, which can represent up to 64% of the flora, and the Staphylococcus aureus, which can account for up to 12 % of the flora, followed by the Micrococciiby other CoNS, by the Propionebacterium, from Corynebacterium. With the use of techniques in molecular biology, these main bacteria have been joined by others such as: Pseudomonas, Bradyrhizobium, Acinetobacter, Brevundimonas,Aquabacterium, Sphingomonas, Streptococcus, Streptophyta, Methylobacterium, Enhydrobacter, Bacillus and Ralstonia spp .
The microbiota plays a very important role, as an ocular surface ecosystem, in the defence against colonisation by other pathogenic germs and creates a balance within it such that opportunistic pathogens do not emerge.
From the above we can deduce that in the mild forms of conjunctivitis, the bacteria that are primarily responsible are generally those forming part of the microbiome that for some reason take over and become pathogenic, thus mainly Staphylococci e Streptococci and much more distant Gram-negatives such as Enterobacteria and Pseudomonas and then the Moraxelle and the Haemophili.
In conjunctival diseases according to the principles of MBSE (Evidence-Based Medicine), taking into account that most bacterial infections tend to be self-limiting within 7/10 days it is type A evidence that in most conjunctivitis (suspected or confirmed) treatment is not necessary. However, it is also type A evidence that the use of topical antibiotics reduces the duration of conjunctivitis, allowing, for example, faster reintegration into work or school, and that it is reasonable to use a broad-spectrum antibiotic to treat the bacterial conjunctivitis.
On the other hand, it is evidence C that in conjunctivitis with mucus-purulent secretion or resistant to therapy, bacterial culture is useful in the first place.
In the case of conjunctival infections in immunocompromised patients, patients with altered adnexa, patients with altered lachrymal film, patients with contact lenses in whom the lesions may evolve, it is advisable to perform before starting therapy the conjunctival smear, which is then examined and interpreted at a reference centre. This is the only way to avoid the indiscriminate use of the latest generation of antibiotics and use those specific to the isolated germ.
In the case of keratitisThere is much debate among clinicians on the use of monotherapy or combination therapy. However, the corneal lesion must always be sampled and analysed using molecular biology techniques and/or a classical technique. Upon identification of the germ and/or antibiogram, therapy should be carried out with the best possible antibiotic against the isolated germ.
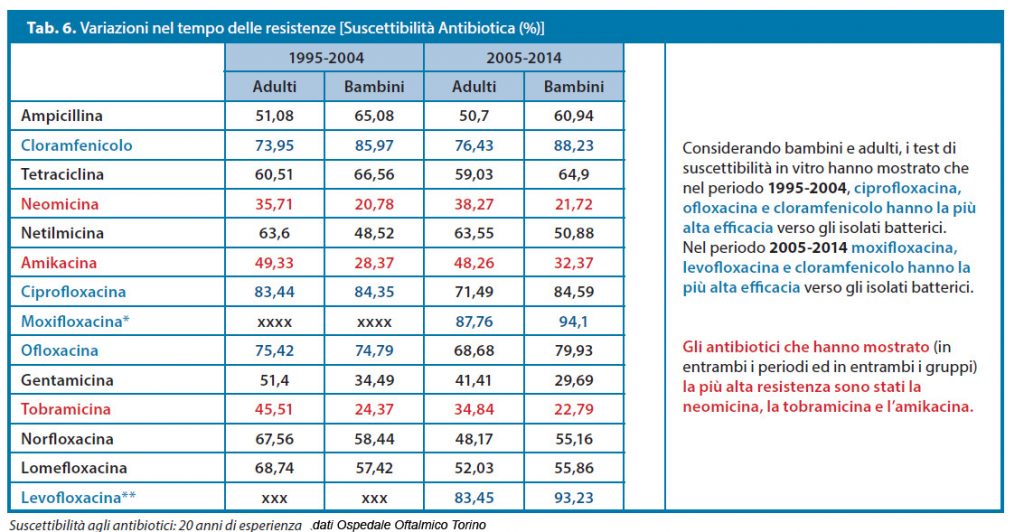
In general, certainly today the greatest concerns come from Growing resistance of CoNS and decreased sensitivity of the Staphylococcus aureus to the older aminoglycosides, but especially to fluoroquinolones.
This means a progressive loss of important weapons against the germs most present in both conjunctivitis and keratitis, and also in the majority of serious eye infections, as together with the problem of methicillin resistance, the problem of multiresistance is becoming increasingly evident.
In this regard, it is important to emphasise the excellent performance of the netilmicin at Staphylococcus aureus methicillin-resistant (MRSA) and on multi-resistant CoNS (MRSE).
Netilmicin is a state-of-the-art aminoglycoside antibiotic, a semi-synthetic derivative of Mycromonospora actynomices. It consists of two amino sugars called garosamines, linked by a hexose nucleus.
Netilmicin is bactericidal and acts by blocking protein synthesis as it binds to the 30S subunit of ribosomal RNA.
Sloane's first publication on the use of this aminoglycoside in endophthalmitis dates back to 1981, and since then there have been more than sixty publications in leading journals concerning netilmycin, in the ophthalmological field in general and topical in particular.
These studies investigate in particular the antimicrobial activity of the drug by assessing bacterial resistance, but also the local tolerability, a very important factor in the choice of a drug for topical use, and the duration of activity of the drug after administration.
Dr. Carmelo Chines
Direttore responsabile
