Microbiota and ocular surface diseases
- In recent years, research has focused on the relationship between the balance of the microbiota and certain ocular surface pathologiessuch as dry eye syndrome, episcleritis, chronic follicular conjunctivitis, pterygium and Thygeson's disease.
All of the aforementioned pathologies are essentially idiopathic in nature, i.e. they are characterised by the absence of an unambiguously identifiable cause, and at the same time are united by the presence of a inflammatory component.
The hypothesis that has guided research in recent years has been that an imbalance in the specific microbiotic community of the ocular surface may determine or contribute to their occurrence, as in the case of the intestinal microbiome and diseases affecting the gut
The ocular surface: the eye's first defence
The ocular surface, under physiologically balanced conditions, constitutes the eye's 'first line' of defence, where many potential attacks, both microbial and environmentally related, are perceived and possibly neutralised.
The first question that has arisen in ophthalmology is whether or not the ocular surface, like other mucous surfaces, has a specific microbiota resident and what role it plays in the physiology of the surface itself.
A study published in 2019 in The Ocular surface illustrated the structure and distribution of the bacterial communities in the different microhabitats of the human eye, mapping their similarities and differences (see Microbiota and the eye - Part I).
In the course of evolutionary processes, therefore, many eubiont micro-organisms, particularly bacteria, have colonised the ocular surface as commensals, playing an important role in maintaining the ocular surface.homeostasi, i.e. the natural tendency to achieve relative stability.
The ocular surface is also equipped with very effective immune defences consisting of active inflammation suppression mechanisms. It is precisely for this purpose that macrophages, dendritic cells, B-cells, IgA, lysozyme, antimicrobial peptides and many other components act as barriers against external agents.
I regular diners of the ocular surface maintain a basic level of activation of innate defences by stimulating epithelial cell receptors.
The normal balance of the ocular microbiota is, therefore, of great importance since pathological infection and inflammation arise precisely when a pathogenic strain infiltrates the ocular flora that can overwhelm the usual flora or a dominant strain secretes an excessive amount of immunogenic substances, such as Staphylococcus exotoxin A, which is among the causes of the onset of marginal keratitis.
Furthermore, the micro-organisms of the microbiota actively participate in the drug metabolism at the level of the mucosa, thus affecting the very effectiveness of drug therapies.
The foregoing attests to the importance of research aimed at understanding the balance of the microbiota from three different perspectives:
- Diagnosisin view of new techniques and tests linking dysbiosis to specific ocular surface diseases.
- Prevention: through probiotic delivery of viable bacterial and microbial strains capable of colonising the surface.
- Treatment: acting on the correction of imbalances in the physiological microbiota, also with a view to favouring the effectiveness of specific pharmacological treatments administered for different diseases.
Dry eye
Dry eye is among the most common ocular pathological conditions, currently affecting tens of millions of individuals worldwide. The origin of this disease is still not entirely clear, but it is believed to be multifactorial. Currently, some of the most promising results in terms of identifying the etiopathological causes come from the multidisciplinary approach, which includes immune-metabolic analysis, microbiota analysis and bioengineering.
Dry eye syndrome or dry eye in medical parlance is referred to as dry keratoconjunctivitis and is a condition that affects the tear film and the ocular surface leading to symptoms of discomfort, visual disturbances, tear film instability with potential damage to the ocular surface.
It is accompanied by an increase inosmolarity (a biochemical parameter related to the number of particles, the osmoles, present) of the tear film and inflammation of the ocular surface.
The tear film
The tear film is a film that covers the corneo-conjunctival surface and forms the direct interface between the eye and the external environment.
It consists of three layers, respectively: lipidic, aqueous and mucous.
The aqueous part of the tear film is the most abundant and contains electrolytes and numerous proteins, including lysozyme, which has specific antibacterial properties. It is produced by the main and accessory lacrimal glands.
The tear film performs numerous functions:
- lubricates the eye, creating a smooth surface on the cornea on which the eyelids can slide easily.
- nourishes the cornea, which, being devoid of blood vessels (avascular), receives nutrients and oxygen precisely through the tear film.
- protects the eye from bacterial and viral infections and removes its waste substances
In the presence of dry eye conditions, both the lachrymal film and the corneo-conjunctival epithelia undergo important changes that, when chronic, are capable of developing phenomena similar to those present during inflammation on the ocular surface.
Dry eye and microbiota
The balance of the ocular microbiota significantly influences the metabolic profile of the ocular surface, which in turn affects the immunity of the surface itself.
Recent studies show that short-chain fatty acids, such as butyrate produced by specific bacteria (such as the Faecalibacterium) play a
Fig. 1. Correlation diagram between microbiota alterations - inflammation - dry eye from Heidari M, , et al. Dry Eye Disease: Emerging Approaches to Disease Analysis and Therapy. Ocul Surf. 2019 important role in Treg (Regulatory T-cell) lymphocyte differentiation.
Similarly, increased populations of Gram-negative bacteria could be responsible for inflammatory responses in dry eye patients, e.g. lipopolysaccharide (LPS), an endotoxin excreted by Gram-negative bacteria, which increases the expression of inflammatory cytokines in the cornea and conjunctiva.
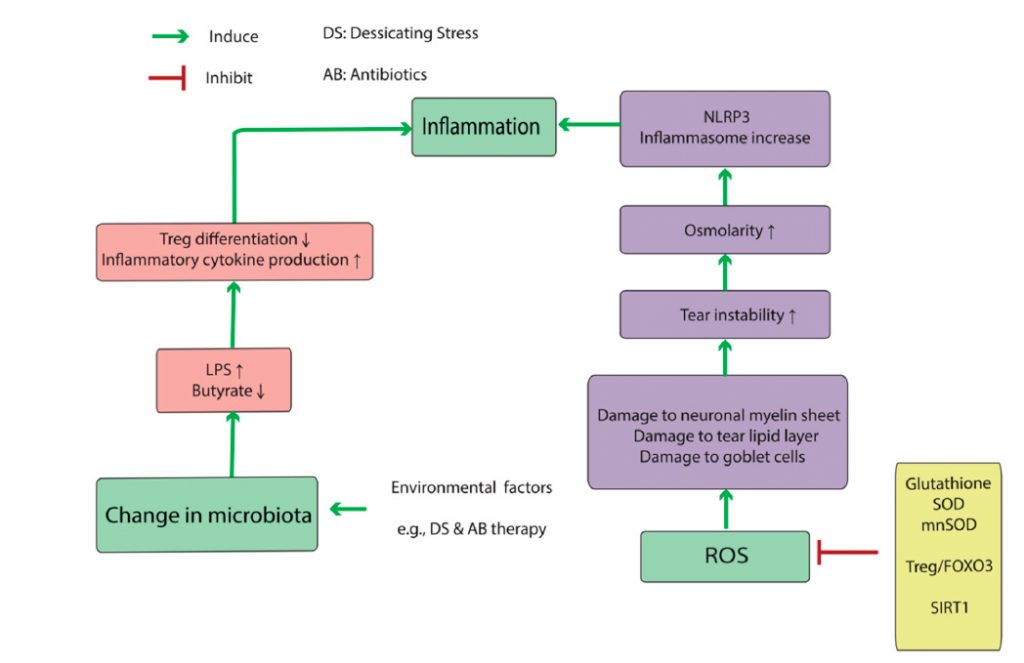
These data suggest that alterations in the normal composition of the microbiota provoke an abnormal immunological response (particularly through immunometabolic mechanisms), which is precisely part of the pathophysiological mechanisms underlying dry eye.
Sources
- Ozkan J, Willcox M, Wemheuer B, Wilcsek G, et al. Biogeography of the human ocular microbiota. Ocul Surf. 2019 Jan;17(1):111-118.
- Heidari M, Noorizadeh F, Wu K, et al. Dry Eye Disease: Emerging Approaches to Disease Analysis and Therapy. J Clin Med. 2019 Sep 11;8(9). pii: E1439.
- Zegans M.E., Van Gelder R.N. Considerations in Understanding the Ocular Surface Microbiome. Am. J. Ophthalmol. 2014;158:420-422.
- Furusawa Y, Obata Y, Fukuda S, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504:446-450.
This article can also be downloaded in PDF format
Sheet No. 7 - Microbiota part 3
© Copyright 'l'Oculista italiano
See also
Sheet no. 6: Microbiota - part 2
Sheet 5: Microbiota - part 1
Dr. Carmelo Chines
Direttore responsabile
