The latest trends confirm the importance of a conscious prescriptive approach.
The ARMOR study (Antibiotic Resistance Monitoring in Ocular microorganisms) has been active in the US since 2009 and promotes a nationwide antibiotic resistance surveillance programme specifically targeted at ocular pathogens.
The latest available data, presented at the 2017 ARVO Congress, may be useful in guiding clinicians' choices in identifying antibiotic therapy to be used for initial empirical treatment and prophylaxis of ocular infections.
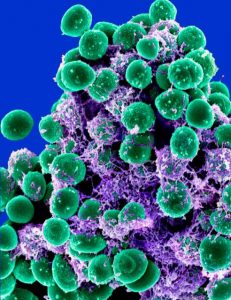
Analysis of the data collected during the first 10 months of 2016 shows that the level of antibiotic resistance continues to be high in staphylococcal isolates and especially among methicillin-resistant (MR) species. Moreover, the rate of multi-resistance of these microorganisms, i.e. resistance to 3 or more classes of antibiotics, remains high especially among MR strains.
As staphylococci are very common pathogens as causes of ocular infections, and starting from the fact that antibiotic resistance rates among these organisms remain high, a trend analysis was also promoted, specifically aimed at identifying changes in resistance of isolates of S. aureus and CoNS (Coagulase Negative) in the 8 years since the ARMOR study began. The analysis included data from 1,597 isolates of S. aureus i and 1,400 CoNS isolates included in the ARMOR study between January 2009 and October 2016.
The results show that the overall rate of methicillin resistance in isolates of S. aureus decreases significantly over time, falling from 39% in 2009 to 27% in early 2016. In contrast, there is no reduction in the methicillin resistance rate in CoNS isolates, with almost half of CoNS isolates being methicillin-resistant in 2016.
Focusing on the data on the isolates of S. aureus, Trend analysis shows significant decreases in resistance rates from 2009 to 2016 for azithromycin (from 62% to 47%), ciprofloxacin (from 39% to 25%), and tobramycin (from 24% to 9%). In CoNS isolates, resistance to ciprofloxacin also decreases significantly over the 8-year period, from 46% in 2009 to 30% in 2016, but CoNS resistance to trimethoprim increases significantly from 26% to 37%.
Commenting on the results of the trend analysis, Dr Penny Asbell, Professor of Ophthalmology at the Icahn School of Medicine and Director of the Cornea and Refractive Surgery Center at Mount Sinai Hospital (New York) said "Over the eight years of the ARMOR study, staphylococci showed a significant increase in resistance rates from the tested species. In recent years, there has been a plateau in resistance rates, which now even appear to be decreasing. We can state that the reduced resistance by S. aureus to methicillin, macrolides, fluoroquinolones and aminoglycosides are promising results, which may reflect an improvement in the management of antibiotic therapy and awareness of the challenges that antibiotic resistance poses to patient health'.
However, the persistence of high resistance rates among CoNS with no change in methicillin resistance and an increase in trimethoprim resistance once again confirm the importance of a prudent approach to antibiotic prescribing in order to limit the development of bacterial resistance to existing treatment options.
Dr. Carmelo Chines
Direttore responsabile
