Vitreous diseases are pathological changes that affect the vitreous body of the eye and lead to vision disturbances related mainly to the presence of floating bodies, with repercussions on the psychological and emotional state of the affected person.
Main non-age-related diseases of the vitreous body
Vitreous diseases may or may not be age-related
Age-related pathologies
Myodesopias e posterior vitreous detachment
Non-age-related pathologies
Haemovitreo
Eye condition characterised by the presence of blood in the vitreous body, due to the rupture, either spontaneous or trauma-induced, of certain blood vessels. Haemorrhages affecting the vitreous can be triggered by the presence of pathologies such as high blood pressure, diabetic pathology and proliferating diabetic retinopathyThe latter is characterised by the uncontrolled formation of new blood vessels with a very weak wall. The symptoms of haemvitreous are not of a painful nature, but are rather characterised by the presence of myodesopias, the floating bodies in the vitreous. In general, over a period of weeks or months, the blood in the vitreous becomes reabsorbs spontaneouslyin other cases, however, the administration of anti-haemorrhagic drugs. In cases where the haemorrhage is associated with a retinal detachment, however, surgery may be the decisive strategy.
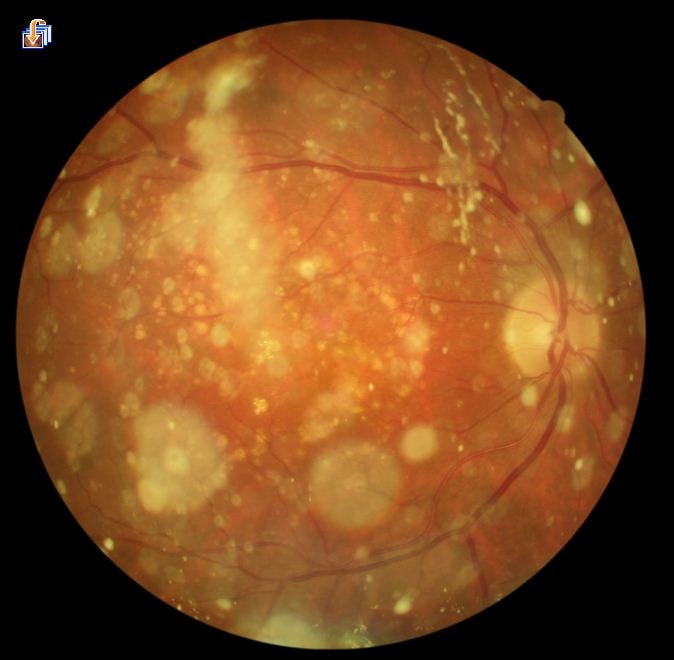
Hyalosis asteroid
Pathology characterised by the formation of spherical agglomerates, known as asteroid bodies, of colour white-yellow and consist mainly of calcium salts and lipids. The formation of these spheres is due to an ageing process of the collagen present in the vitreous body and, in fact, occurs in the over 60s population. The triggering factors are not yet fully known, but clinical data have shown a higher prevalence of this visual disorder in conjunction with certain diseases such as diabetes, arteriosclerosis and hypertension. Asteroid hyalosis is asymptomatic and uncomplicated, so it is generally only discovered after an eye examination.
Sparkling synchysis
It affects the people of a young age (under 35 years), and is due to the appearance of numerous crystalline, shiny, flat-shaped corpuscles. These corpuscles are suspended in the vitreous body and move following the movement of the eyes. It can occur as a result of trauma, chronic inflammation or without any known or apparent cause (idiopathic form).
Primary hyperplastic vitreous
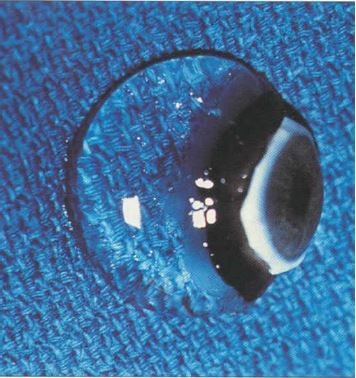
Very rare congenital pathology which occurs when, at birth, the correct regression of the primary vitreous body and the halo-dea vasculature normally only present in the foetus does not take place. In a normal physiological process, from as early as the second month of gestation, the regression processes of the primary vitreous begin to be activated to make room for the secondary vitreous; if this does not occur, or occurs incompletely, two forms of hyperplastic vitreous can occur depending on the ocular structures involved: anterior and posterior. The presence of hypertrophic primary vitreous at birth is the most common cause of cataracts in children, as well as glaucoma and retinal detachment.
Diagnosis
The diagnosis of degeneration of the vitreous body is made through acareful anamnesis of the patient and depends on the stage of the pathology.
The ophthalmologist, in fact, carefully assesses the history of the affected person to first understand whether the causes are  ocular or not directly related.
ocular or not directly related.
The next step is to carefully ocular fundus examination.
Comprehensive ocular diagnostics include:
- Field of vision
- Pupillary response for relative afferent pupillary defect (RAPD)
- Visual acuity
In most cases, a direct ophthalmoscopy is performed, but this alone may be insufficient because the retinal tears that occur as a result of the retinal fissure are located in the periphery and this technique is not always able to detect them.
Treatment
If the vitreous pathology is not at an advanced stage and the retina is not compromised, no real treatment is required. In fact, the main symptoms of the changes affecting the vitreous, the myodesopias, tend to fade as the months go by because the brain gets used to their presence.
In these cases, the most commonly used strategies include the use of food supplements capable of reducing the symptoms associated with these alterations. In particular, supplements based on collagen, calcium, vitamins, hyaluronic acid and glycosaminoglycans are recommended that can improve connective tissue trophism.
If the vitreous pathology worsens and the symptoms do not subside spontaneously or with the use of specific supplements, surgical treatment may be required.
Vitrectomy
In the most severe clinical cases, vitreous degeneration requires surgery, the vitrectomythrough which it is degenerated vitreous gel is removed and replaced with an artificial one. Although vitrectomy is a decisive operation, especially in the most severe cases, it may be responsible for the occurrence of certain complications, including cataracts, retinal detachment, ocular inflammations/infections or ocular haemorrhages, and for this reason ophthalmologists tend to perform this type of operation as a last resort.
YAG laser vitreolysis
Recently, in order to minimise the occurrence of complications, a number of techniques have been introduced, including the YAG laser vitreolysis. With this technique, myodesopias are hit, vaporised or moved away from the field of view by the use of a laser light beam. Vitreolysis it is neither invasive nor painful and is performed in an outpatient setting in about 20 minutes using only a topical anaesthetic. Although the procedure is safe and almost free of contraindications, it cannot be applied if the movable bodies are located near the macula, the central area of the retina responsible for central vision.
- Kahawita S. et al. Aust Fam Physician, 43 (4): 201-3, 2014. Flashes and floaters- a practical approach to assessment and management.
- The vitreous body and related pathologies. L'Oculista Italiano. Year XLVII - March 2016
