The correct differential diagnosis is essential to direct the patient with viral conjunctivitis towards the most appropriate treatment, in order not to risk the incorrect use of antibiotics.
Conjunctivitis: classification
The conjunctivitis is a very common inflammation of the conjunctiva, which can affect individuals of all ages.
Conjunctivitis is one of the most common diseases of the anterior segment of the eye.
It is an inflammation of the conjunctiva, the transparent mucous membrane that covers the anterior portion of the eyeball, with the exception of the cornea, and the inner wall of the lower and upper eyelids, up to the lid margin.
Conjunctivitis can be caused by:
1) Biological agents (bacteria, viruses; mycetes; parasites);
2) from physical agents (e.g. ultraviolet radiation or thermal radiation);
3) from chemical agents (e.g. cosmetics or drugs);
4) from environmental factors (e.g. smoke or dust).
There are also allergic and/or immune-mediated conjunctivitis and conjunctivitis due to an alteration of the tear film.
Of the different types of conjunctivitis, viral conjunctivitis is the most common, accounting for up to 75% of cases.
Viral conjunctivitis
Adenovirus is the most frequent cause of viral conjunctivitis. It has numerous different serotypes, which can cause different clinical pictures. Virus transmission occurs by direct inter-human contact, by air via saliva droplets, or by infected instruments. The incubation period is 5 to 12 days, the disease 5 to 15 days, and there are three typical presentations:
1. Acute conjunctivitis follicularis:
2. Pharyngoconjunctival fever
3. Epidemic keratoconjunctivitis:
Symptoms of viral conjunctivitis include:
- reddening
- congestion of blood vessels,
- ocular secretion
- pain
- photophobia
- pseudomembranes.
Antibiotic treatment
The prescription of antibiotics in cases of viral conjunctivitis represents one of the biggest costs in any health care system.
For example, the percentages of patients with infectious conjunctivitis treated with antibiotics in the UK vary between 80% and 95%.
While the improved diagnosis of viral conjunctivitis is estimated to have reduced the inappropriate prescription of antibiotics and saved $430 million per year in the US.
Clinical studies are currently underway to evaluate specific treatments for conjunctival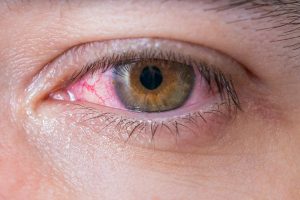 ite viral.
ite viral.
Due to the non-specificity of signs and symptoms of this type of conjunctivitis, a comprehensive history with clinical examination is necessary, especially in patients with atypical signs and a chronic course.
Aetiology of viral conjunctivitis
Viral conjunctivitis can be caused by adenoviruses, herpes viruses and, as seen recently, can also lead to burning eyes due to coronaviruses such as SARS-CoV-2.
- Adenoviruses are viruses of the Adenoviridae family, with double-stranded DNA and no envelope. Infections frequently associated with adenoviruses include upper respiratory tract and eye infections, and diarrhoea in children. Viral conjunctivitis can be transmitted by direct contact with the virus, by air or by contact with places that act as reservoirs, such as swimming pools.
- Herpes conjunctivitis is common in adults and children and is associated with follicular conjunctivitis. Herpes simplex virus (HSV) is estimated to be responsible for 1.3-4.8% of cases of acute conjunctivitis.
- Varicella-zoster can also cause conjunctivitis, through direct eye contact or skin lesions or inhalation of infected aerosolised particles, especially with involvement of the first and second branches of the trigeminal nerve.
- Picornavirus EV70 and the coxsackievirus variant A24 (CA24v) are, on the other hand, the pathogens responsible for acute haemorrhagic conjunctivitis (AHC), a highly contagious form of viral conjunctivitis whose symptoms include foreign-body sensation in the eye, epiphora, eyelid oedema, conjunctival chemosis and subconjunctival haemorrhage.
- Finally, it has been reported that the recently isolated SARS-CoV-2 coronavirus strain can also cause conjunctivitis. Retrospective and prospective studies show that 1% to 6% of patients show COVID-19-related conjunctivitis, with positive conjunctival swabs in 2.5% of cases.
Treatment and management of viral conjunctivitis
Treatment for viral conjunctivitis is aimed at symptomatic relief and not eradication of the infection, which is generally self-limiting.
Resolution of conjunctivitis can take up to three weeks and treatment includes the use of artificial tears to lubricate the eye.
Cold compresses with a damp cloth in the eye area can also provide symptomatic relief and have the advantage of not constituting a pharmacological treatment.
The use of iodine-povidone, a non-specific disinfectant, is a promising new treatment for adenoviral conjunctivitis. It is a cheap and widely available antiseptic, which is used as part of the aseptic preparation for eye surgery. It is able to kill extracellular organisms but has no intracellular effect. Moreover, it does not induce drug resistance because its mechanism of action is not immunologically dependent.
Treatment with antibiotic drops is not helpful in cases of viral conjunctivitis and, indeed, can potentially increase bacterial resistance and the formation of pseudomembranes, which subsequently require removal to reduce discomfort and scarring.
Prevention and patient education
In addition to treatment, it is necessary to prevent the spread of the infection to the other eye or to other people, so the patient must be educated to practise good hand hygiene with frequent hand washing, avoiding sharing towels or sheets, and avoiding touching the eyes.
As seen, the vast majority of viral conjunctivitis is caused by adenoviruses and
Frequent handwashing, disinfection and isolation of patients with conjunctivitis can reduce further transmission in the community.
Long-term sequelae are rare, however chronic viral conjunctivitis can lead to a poor quality of life. In most cases, one to four weeks are required to recover without treatment.
Complications are not common, but may include corneal ulceration and punctate keratitis.
See also:
- Netilmycin/dexamethasone in the treatment of conjunctivitis - Oculist Italiano
- Treatment of neonatal chlamydia conjunctivitis - Oculista Italiano
Dr. Carmelo Chines
Direttore responsabile
