L'hyaluronic acid is a high molecular weight polyanionic polysaccharide with a typical spiral structure that gives it a particular ability to combine with water1 and an excellent viscoelasticity.
This results in an excellent moisturising capacity and a pronounced pseudoplastic behavioursimilar to that of the soluble mucins in the tear film.
What pseudoplastic means
In fluid mechanics, 'pseudoplastic' is said of non-Newtonian fluids in which the coefficient of viscosity decreases as shear stress increases.
In the case of hyaluronic acid contained in eye drops, 'pseudoplastic' means that it has a higher viscosity when the eye is open and a lower viscosity during blinking, allowing lubrication of the entire ocular surface.
Properties
The properties Hyaluronic acid's ability to bind large amounts of water and its ability to mimic the behaviour of mucins help to maintain the stability of the tear film (3) and ensure optimal ocular protection and lubrication. In addition to these particular properties, hyaluronic acid also plays an important biological role in the processes of corneal repair (4), promoting cell motility, adhesion and proliferation.
Recent studies have also shown that these characteristics are complemented by hyaluronic acid's ability to limit the damaging effects on the ocular surface due to the chronic use of ophthalmic products containing benzalkonium chloride (BAC) (5).
Benzalkonium chloride
The Benzalkonium chloride is a quaternary ammonium compound with cleansing properties, commonly used in ophthalmic preparations as a preservative for its high antimicrobial power e high stability.
Chronic use of products preserved with BAC may, however, alter the integrity of the cellular lipid membranes of the corneal epithelium due to its cationic nature6. The interaction of BAC with cell membranes may also lead to an increase in extracellular Adenosine Triphosphate (ATP) that is highly affinitive to P2X receptors75.
The latter are part of a family of transmembrane receptors consisting of subunits, the aggregation of which forms ion channels that mediate the entry of low molecular weight cations such as sodium and calcium into the cell and the escape of potassium. The P2X7 receptor recognises several nucleotides as ligands and is mainly activated by the nucleotide ATP. Activation of this receptor by high concentrations of ATP leads to the formation of cytolytic pores and a series of intracellular events that culminate in cell apoptosis (7,8,9).
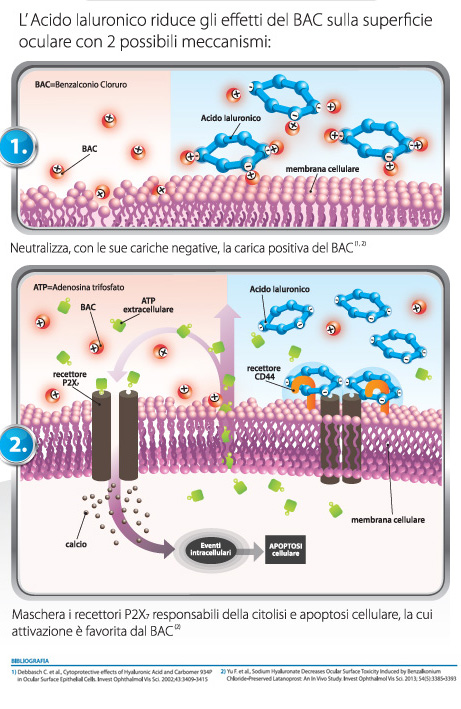
The protective action on the ocular surface shown by hyaluronic acid during chronic treatment with ophthalmic products containing BAC has been attributed to two different mechanisms.
A direct mechanism (Fig. 1), whereby hyaluronic acid is able to neutralise the positive charge of BAC thanks to its numerous negative charges5,10, and an indirect mechanism (Fig. 2), whereby hyaluronic acid binds to its specific CD44 receptors, masks P2X7 receptorswhose activation is favoured by BAC. This therefore does not allow the intracellular events that lead to cell apoptosis to be triggered (5,7,8,9).
Dry eye after cataract surgery
Senile cataract is an age-related eye disease for which the treatment of choice is phacoemulsification combined with intraocular lens implantation. Ocular surface diseases are common after cataract surgery and can have a negative impact on patients' quality of life. In addition, the use of anti-inflammatory eye drops before cataract surgery can often cause damage to the epithelium and, subsequently, the alteration of the tear film due to the surgery can lead to an increase in local inflammatory factors. Finally, the corneal incision causes damage to the epithelial cells of the cornea and local anaesthesia can also cause discomfort to the ocular surface after surgery.
All these factors are among the causes contributing to the onset of dry eye after cataract surgery. Moreover, with advancing age, both cataract and dry eye syndrome (which is the most common ocular surface disease) have a higher incidence. To reduce patients' discomfort, it is therefore important to find suitable treatments to lessen the impact of cataract surgery on the ocular surface.
Among the most interesting substances in this respect is the sodium hyaluronate, the sodium salt of hyaluronic acid, a molecule capable of retaining water on the ocular surface and retarding evaporation of the tear film. A recent study investigated ocular surface changes after phacoemulsification in patients with age-related cataracts following the addition of drops with varying concentrations of sodium hyaluronate.
Conduct and design of the study
Nello studioThe authors examined the efficacy of 0.3% and 0.1% sodium hyaluronate eye drops in restoring the regularity of the corneal surface in patients who developed dry eye syndrome after cataract surgery. The drops were administered topically four times a day in 73 patients, divided into three groups: in group A, 30 patients received conventional therapy and 0.3% sodium hyaluronate eye drops; in group B, 31 patients received conventional therapy and 0.1% sodium hyaluronate eye drops; in group C, only conventional therapy was administered in 30 patients. Conventional postoperative therapy included eye drops with levofloxacin and tobramycin dexamethasone, both administered four times daily, and eye drops with bromfenac sodium, administered twice daily. Evaluations were performed at specific intervals up to 3 months postoperatively and included assessments of tear film stability and irregularity.
Patients were then examined seven days, two weeks, one month and two months after surgery and significant differences were found in the Schirmer I test, tear film meniscus height and tear film break-up time values in both groups treated with sodium hyaluronate, compared to controls. Furthermore, the 0.3% concentration gave even better results two months after surgery. Corneal irregularity values also decreased more significantly in the 0.3% sodium hyaluronate treatment group, compared to the 0.1% sodium hyaluronate treatment group and the control group.
What are the implications of the study for clinical practice?
Overall, the study showed that sodium hyaluronate is able to restore tear film structure and corneal surface regularity, and that the 0.3% concentration is more effective than the 0.1% concentration. Thus, in the initial phase after phacoemulsification, where tear film stability is reduced, hyaluronate drops are an excellent choice for maintaining ocular surface health.
The authors state that further prospective and comparative studies including patient-reported outcomes will be needed to establish with even greater certainty the role of sodium hyaluronate in the management of patients who develop dry eye disease after cataract surgery. However, pending such further confirmation, sodium hyaluronate eye drops may be considered a useful therapeutic option for patients with dry eye symptoms after cataract surgery.
Dr. Carmelo Chines
Direttore responsabile
- 1. Nakamura M. et al, Characterization of Water Retentive Properties of Hyaluronan. Cornea 1993;12(5):433-436.
- 2. Laurent T.G. et al., Hyaluronan. PHASEB J. 1992;6:2397-2404.
- 3. Lee J.H. et al., Efficacy of Sodium Hyaluronate and Carboxymethylcellulose in Treating Mild to Moderate Dry Eye Disease. Cornea 2011;30:175-179.
- 4. Camillieri G. et al, Hyaluronan-induced stimulation of corneal wound healing is a pure pharmacological effect. J Ocular Pharm Ther 2004;20(6):548-553.
- 5. Yu F. et al, Sodium Hyaluronate Decreases Ocular Surface Toxicity Induced by Benzalkonium Chloride-Preserved Latanoprost: An In Vivo Study. Invest Ophthalmol Vis Sci. 2013;54(5):3385-3393.
- 6. Okahara A. et al, Local toxicity of benzalkonium chloride in ophthalmic solutions following repeated applications. J Toxicol Sci 2013;38(4):531-537.
- 7. Dutot M. et al, Fluoroquinolone Eye Drop-Induced Cytotoxicity: Role of Preservative in P2X7 Cell Death Receptor Activation and Apoptosis. Invest Ophthalmol Vis Sci. 2006;47(7):2812-2819.
- 8. Dutot M. et al, Effects of toxic cellular stresses and divalent cations on the human P2X7 cell death receptor. Mol Vis. 2008;14:889-897.
- 9. Adinolfi E. et al., Basal activation of the P2X7 ATP receptor elevates mitochondrial calcium and potential, increases cellular ATP levels, and promotes serum-independent growth. Mol Biol Cell 2005;16:3260-3272.
- 10. Debbasch C. et al, Cytoprotective effects of Hyaluronic Acid and Carbomer 934P in Ocular Surface Epithelial Cells. Invest Ophthalmol Vis Sci. 2002;43:3409-3415.