Maculopathies and the latest developments in medical therapy are the focus of our interview with Dr. Monica Varano, Head of the Retina Medica Service at IRCCS Fondazione Bietti, one of Italy's most qualified opinion leaders in the field of medical retina.
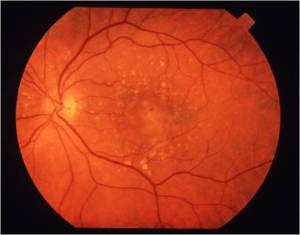
[caption id="attachment_751" align="alignleft" width="300" class=" "] Colloid macular degeneration[/caption]
Colloid macular degeneration[/caption]
Should we expect news on the pharmacological level, also related to the EMEA's approval at the end of 2012 for the use in European countries of VEGF-Trap drugs, such as Aflibercept (approved at the recommended dose of 2 mg for every other month after the loading phase)?
Certainly Aflibercept represents a very interesting drug. The result of one-year comparison studies showed that the efficacy and safety of Aflibercept (EYLEA), injected every 2 months after the loading dose.
This treatment scheme, which is more programmable and requires less close monitoring, could be less burdensome for the patient, carers and ophthalmologist, especially at a time when centres dealing with maculopathies are overwhelmed by a huge volume of patients who have to be monitored and retreated continuously.
What are the long-term prospects for patients undergoing intravitreal treatment, first and foremost on a clinical level?
The data available to us on long-term treatment show, due to the characteristics of the disease, the need to continue close monitoring even after the second year and to retreat the patient as needed, otherwise the possibility of visual decrement has been demonstrated.
Regarding safety, repeated injections of Ranibizumab proved to be well tolerated for a period of more than 4 years.
[caption id="attachment_752" align="alignright" width="300" class=" "] Exudative macular degeneration[/caption].
Exudative macular degeneration[/caption].
What do you think of the SOI's official position supporting the off-label use of intravitreals in young patients (over 1 million in Italy alone) with myopic maculopathy versus on-label photodynamic therapy?
The case of neovascularisation in the myopic subject is very special because there is so much evidence from the literature absolutely all agreeing that anti-VEGF therapy is superior to photodynamic therapy (which is the one currently recognised for this indication) that at the moment, even in the absence of more important scientific evidence results (randomised controlled clinical trials-RCTs) the use of off-label anti-VEGF (Bevacizumab, Ranibizumab) is absolutely advisable.
A very brief mention of the rationale for nutritional therapy, particularly with reference to the case of the contralateral eye in patients already suffering from the wet form, do you agree with its use?
I would like to share this. Evidence on the effectiveness of antioxidant vitamin and mineral supplementation was demonstrated in the AREDS study. AREDS I-type supplementation has been shown to reduce the risk of developing the advanced form of AMD by 25% in people at intermediate risk of the disease or with advanced AMD. In a small multicentre study conducted in Italy a few years ago (Carmis study), patients treated with lutein 10 mg, zeaxanthin 1 mg, astaxanthin 4 mg, vitamin C 180 mg, vitamin E 30 mg, zinc 22.5 mg, copper 1 mg, were more likely to report clinically significant stabilisation and/or improvements in visual acuity, contrast sensitivity, and selective dysfunction in the central retina (0 degrees -5 degrees), measured by multifocal erg, was improved at 12 months compared to untreated subjects.
[caption id="attachment_753" align="alignleft" width="300" class=" "]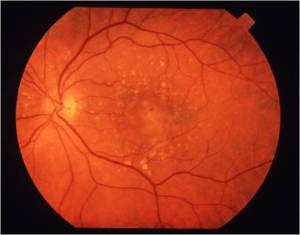 Exudative macular degeneration[/caption].
Exudative macular degeneration[/caption].
Lutein supplementation was found to be protective against the disease, according to recent results of the AREDS2 study recently reported at the ARVO congress in Seattle. Exactly in the AREDS2 study, the addition of DHA/EPA or lutein/zeaxanthin to the original AREDS formulation (which contained beta-carotene) had no overall additional effect on the risk of advanced AMD. However, participants who took the AREDS formulation containing lutein/zeaxanthin and not beta-carotene had a slight reduction in the risk of advanced AMD, compared to those who took the AREDS formulation with beta-carotene (which was also found to be dangerous for ex-smokers due to the risk of lung cancer). Furthermore, for a subgroup of participants with very low levels of lutein/zeaxanthin in their diet, the addition of these supplements to the AREDS formulation helped reduce their risk of advanced AMD.
A final question related to a topic you have recently dealt with: macular sensitivity assessed by Microperimetry in various maculopathies, in particular macular sensitivity in patients with lamellar holes, would you summarise for us the latest advances in scientific knowledge on this subject?
Microperimetry is an examination that offers the possibility of carrying out a study of fixation (stability and localisation) and the retinal sensitivity threshold through direct real-time visualisation of the ocular fundus. It is a very useful diagnostic examination in certain types of macular pathologies of a degenerative or dystrophic nature and of fundamental importance in the management of pathologies that affect the vitreo-retinal interface (cellophane, pucker, pseudopores and macular holes). It is mainly used to monitor a disease, to check the results of a therapy, to obtain a morpho-functional approach compared with OCT. Recently, we evaluated the macular sensitivity of patients with lamellar macular holes with microperimetry to explore the relationship between macular function, anatomical features of the lamellar hole and vitreal status.
This study showed that visual acuity and retinal sensitivity are reduced in the lamellar hole and that this reduction correlates neither with diameter nor with residual foveal lamellar thickness. Conversely, the reduction in retinal sensitivity appears to be influenced by the depth of the defect. Furthermore, impaired macular function is more pronounced in eyes with abnormalities of the outer retinal layer.
Dr. Carmelo Chines
Direttore responsabile