Find out what the main visual tests for diagnosis are.
What is an eye test
A comprehensive eye examination consists of three fundamental moments:
1. Medical history: which consists of the collection from the direct voice of the patient and/or his/her family members (e.g. parents in the case of an infant or child) of information relating to the patient's ocular and systemic, personal and family history and condition.
2. Ophthalmic or visual test: clinical and instrumental examination to assess the anatomical condition and function of the eyes and ocular adnexa.
3. Evaluation of diagnostic findings, formulation of a diagnosis e prescription of a possible therapy.
The main visual tests
- External inspection or direct examination
- Slit-lamp examination or corneal biomicroscopy
- Refraction examination
- Measuring thevisual acuity for far and near
- Examination of contrast sensitivity
- Examination of the colour sense
- Examination of the ocular fundus or ophthalmoscopy
- Tonometry
- Pachymetry
- Perimetry or Field of View
– FAG, ICGA and OCT
- Electrophysiological examinations
- Testing of dark adaptation (adaptorometry)
- Autofluorescence measurement
External inspection or direct examination
This eye test, carried out with the naked eye or with the aid of a pocket lamp and a magnifying glass, is used to detect obvious abnormalities of the eyelids, conjunctiva, cornea, pupil, iris and eyeball (e.g. exophthalmos).
Slit-lamp examination or corneal biomicroscopy
The slit lamp is a special binocular microscope, which rotates around a pivot so that the eye can be inspected, particularly the front segmentfrom different angles. It is equipped with a light source, also movable, whose beam has the shape of a slit (hence the name of the instrument) and an adjustable intensity, so that the eye can be examined through different 'optical sections'.
The slit lamp also allows examination of the rear segmentof the vitreous and the ocular fundususing the Goldmann contact lenswhich is placed on the eye under topical anaesthesia. This lens is flat on the side facing the doctor and concave on the opposite side to adapt to the curvature of the cornea. This eliminates the strong refractive power of the cornea and allows the physician to examine the posterior segment with the microscope.
Inside the contact lens are several mirrors that allow the most peripheral parts of the retina to be seen through the pupil. One of these mirrors also allows one to examine theirido-corneal angle. In recent years, the use of non-contact lenses has become widespread, Volk lenses and similar, to be manually inserted into the beam path of the slit lamp, which provide an excellent view of the background up to almost the extreme periphery.
Refraction examination
The refractive eye test includes:
- The measurement of refractive errors o refractometrywhich can be carried out using objective methods such as the schiascopia traditional or strip, or subjective/objective using the autorefractometers.
- The optical correction, which consists of the ophthalmologist prescribing the most appropriate lens for focusing light rays on the retina.
The ophthalmologist uses the eye prescription in which all the necessary data is entered so that the optician can provide the patient with the correct spectacles for the correction he or she needs.
Certain abbreviations are often used in ophthalmic prescriptions, such as:
- ADD (Addition): indicates the additional power in multifocal or progressive contact lenses (expressed in diopters). In most cases the value can vary from a minimum of +1.00 to +3.00.
- AX (Axis): is the position of astigmatism in degrees. The value ranges from 0 degrees to 180.
- BC (Base Curve) or RB (Base Radius): corresponds, using the unit of measurement in millimetres, to the curvature of the ocular lens.
- CYL (Cylinder) or CIL (Cylinder): Indicates the area of the lens called the cylinder. In toric lenses, the CIL indicates the power of the lens to correct astigmatism, expressed in diopters
- OD (Right Eye) or RE (Right Eye)
- OS (Left Eye) or THE (Left Eye)
- DDioptria.
The Diopter, in optics, is the unit of measurement (in m-1) of the refractive power of an optical system or lens and expresses its ability to change the directions of incoming light rays to focus and translate them into an image at a certain distance from the centre of the optical system itself (focal distance). The number of diopters of a lens or optical system is equal to the inverse of the focal distance expressed in metres: D = 1/f (m).
In addition, the prescription may be entered under the headings:
- BY DISTANCE: in this case, the glasses should not be used for proximal distances
- FOR NEARBY (or FOR READING): distinguishes glasses for reading only or for proximal distances, to be removed when looking up
- PERMANENCE: corresponds to prescriptions for which the correction must always be in use, for all the distances at which one looks.
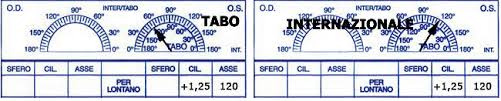
Finally, angular orientations in cylindrical corrections can be rotated according to two different systems:
- The TABO system has the value zero towards the right side of the semicircle depicted
- The INTERNATIONAL system has the zeros placed both nasally
Measurement of distance and near visual acuity
L'visual acuity (Visual Acuity - VA) is the ability to discriminate fine spatial details. Its measurement is based on the reciprocal of theminimum angle of resolutionwhich is the minimum visual angle at which two separate points are still recognisable. It must be preceded by therefraction examination o refractometry and the correction of any defects that would affect its measurement.
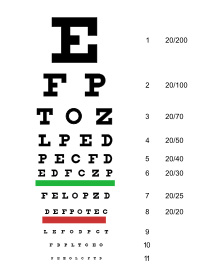
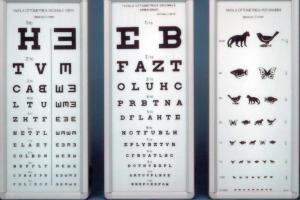
L'distance' visual acuity (VA Distance) is measured using octotypes of various types, i.e. tables containing a series of letters or other graphic signs, to be recognised at a predetermined distance, which is 5 m in Latin and Germanic countries and 20 feet (6 m) in Anglo-Saxon countries. At this distance, the rays coming from the table are considered parallel and, therefore, not activating the accommodative reflex for near.
The most common octotypes in Europe are the decimal ones, type Armaignacwhile in Anglo-Saxon countries the Snellen table (reading distance 20 feet).
Next to or above each row of characters in the optotype a fractional number indicates the visual acuity. On the decimal scale, a healthy subject will have a visual acuity of 10/10, which means that the 10th line of the optotype can be at a distance of 5 m.
The octotypes should have standard illumination or rather be self-illuminated, since visual acuity depends on the intensity of illumination.
For each eye, both the natural visus (uncorrected visual acuity) and the visus with possible correction.
L'near' visual acuity is measured with tables containing literal text or a series of numbers or, for children, drawings of common objects. The reading distance is 33 cm (13 inches), the measurement is usually expressed in typographic "dots" and the visual acuity is normal when text is read at the distance indicated by D to the left of each character size.
[caption id="attachment_554" align="aligncenter" width="300"]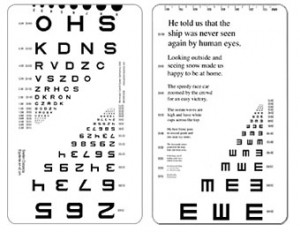 Octotype board for neighbour Wormington[/caption].
Octotype board for neighbour Wormington[/caption].
Examination of contrast sensitivity
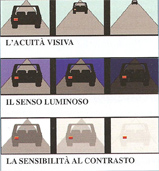 The overall assessment of the quality of vision of a patient is based not only on the determination of visual acuity, but also on the luminous sense, which is the ability to distinguish poorly lit objects, and the contrast sensitivitywhich is the ability of the retina to perceive differences in illumination between an object and the background. Even with perfectly normal visual acuity, visual function can sometimes be significantly impaired precisely because of reduced contrast sensitivity.
The overall assessment of the quality of vision of a patient is based not only on the determination of visual acuity, but also on the luminous sense, which is the ability to distinguish poorly lit objects, and the contrast sensitivitywhich is the ability of the retina to perceive differences in illumination between an object and the background. Even with perfectly normal visual acuity, visual function can sometimes be significantly impaired precisely because of reduced contrast sensitivity.
To measure contrast sensitivity, special octotype tables are used, in which the relative brightness between the character and the background varies (e.g. Pelli-Robson Tables) or gridsi.e. stimuli consisting of alternating light and dark parallel bars or sine bars. All these tests can often be performed by means of computerised octotypes.
Contrast sensitivity is expressed not with a number, but with a curve.
Examination of the colour sense
The eye test of the colour sense allows the ability to recognise the three basic colours: red, green and blue.
They are used to diagnose colour sense defects, both congenital and acquired.
[caption id="attachment_556" align="alignleft" width="300" class=" "]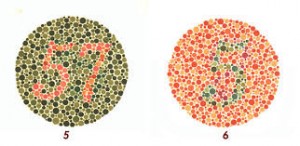 Tables of Ishiara[/caption]
Tables of Ishiara[/caption]
The main tests are:
1. Naming or comparison testsduring which the patient is asked to recognise and name objects of the same colour (skeins, balls, etc.) or lights that can be monochromatic or multicoloured.
2. Pseudo isochromatic testsin which the patient has to identify a coloured object (number, letter or geometric figure) within particular mosaic boards. The most commonly used are the Ishihara tables, with mosaics made up of coloured and grey discs. The patient with normal colour vision will be able to perceive the numbers or symbols represented in them.
3. Visual classification testsin which the patient has to rearrange coloured tablets into correct colour sequences within a maximum time. The most commonly used are the Fansworth 16 HUE test (used in children as young as 4 years of age, illiterates and those with very low visual acuity) and 100 HUE.
Examination of the ocular fundus (ophthalmoscopy)
The examination of the ocular fundus is performed with the ophthalmoscope, which can be direct or indirect. For a good stereoscopic view of the posterior segment, the pupil must be dilated pharmacologically through the instillation of a few drops of an eye drops midriatic (i.e. able to dilate, in about 15-20 minutes).
The mydriasis prevents the patient from seeing close up and reduces light tolerance; vision usually returns to normal within a few hours. The structures that are thus examined are: the optic papilla, the macula, the retinal vessels, the periphery of the retina and any pathological findings (oedema, haemorrhages, pigment changes, etc.).
Tonometry
Tonometry is an eye test used to detect the "ocular tone', i.e. the internal pressure of the eye (IOP: intraocular pressure), which depends on a delicate balance between the continuous flow of aqueous humour into the anterior chamber and its outflow through the trabecular system.
Normal intraocular pressure values fluctuate in the range of 15 ± 3 mmHg (millimetres of mercury). It may be advisable to repeat the measurement several times during the day to obtain a 'tonometric curve', i.e. a description of the eye pressure trend during the day.
Instruments for measuring intraocular pressure are called tonometers and there are numerous types. At applanation tonometry Intraocular pressure is derived from the mechanical force that is required to flatten a small circular area of the cornea in the central zone.
The Goldmann applanation tonometry is currently considered the gold standard and is the most widely used method in clinical practice. Since, in this case, the tonometer probe comes into contact with the cornea, it is necessary to instill a few drops of an anaesthetic eye drops on the ocular surface. The variability of corneal thickness can in some cases distort the test result, so the values obtained must be corrected with the data obtained through central pachymetry.
Other methods include the non-contact tonometry (o air-jet tonometry) that uses a pulse of air, directed towards the corneal surface, to rapidly applanate the cornea. Intraocular pressure is assessed by measuring the force of the air jet at the instant the applanation occurs. With this technique, the instrument does not come into contact with the eye, thus avoiding the risk of injury or corneal infection. However, some specialists consider non-contact tonometry to be less accurate than applanation tonometry, and therefore, although it is a quick and easy way to measure intraocular pressure, it has been mainly reserved for screening campaigns.
Modern non-contact tonometers have, however, been shown to correlate well with the measurements given by Goldmann tonometry and have proven particularly useful for measuring intraocular pressure in children and other poorly co-operating patients.
Pachymetry or corneal tomography
Pachymetry or corneal tomography is the test used to measure the corneal thickness. This parameter makes it possible to assess the reliability of the intraocular pressure value measured by tonometry: in fact, a thicker-than-normal cornea tends to give higher tonometric values than the actual ones, while on the contrary, a very thin cornea tends to give lower values than the actual ones.
Pachymetry is specifically used for the diagnosis of corneal pathologies such as keratoconus and thecorneal oedema.
The different techniques include corneal tomography with Scheimpflug camera (optical pachymetry), which provides a pachymetric map of the cornea, or via a ultrasound probe (acoustic pachymetry). When using an ultrasonic pachymeter, an anaesthetic eye drops are instilled into the eye before the probe is placed on the corneal surface. The measurement can be repeated at various points on the corneal surface. At the beginning of the test, the patient stares at a light source continuously for a few seconds, during which the instrument performs a series of corneal scans. A dedicated computer performs the morphological and morphometric analysis, extracts the pachymetric value detected at various points of the corneal surface and the minimum corneal thickness value detected.
Perimetry or Field of View
The perimeter or visual field examination is an eye test to assess thewidth of the perceived visual space. It serves to diagnose any field of view defects (visual field alterations), which may be caused by glaucoma, diabetes or retinal degenerative diseases. In the case of glaucoma, in particular, perimetry is very important both for diagnosis and for monitoring the progression of this serious pathology. In fact, the patient's perception of peripheral narrowing of the visual field (the so-called "telescope vision") only occurs long after the actual onset of glaucoma.
Perimetry is a non-invasive eye test, but requires some cooperation from the patient.
One eye is examined at a time. A light stimulus of varying shape and intensity is projected onto the dome with a white background. The patient has to press a button each time they perceive the stimulus. At the end of the examination, a graph is made showing any points or areas of narrowing of the visual field. The examination in both eyes takes about 20 minutes and the results are available immediately.
Today, computerised equipment is used to examine the visual field (computerised perimetry) that allow high diagnostic accuracy.
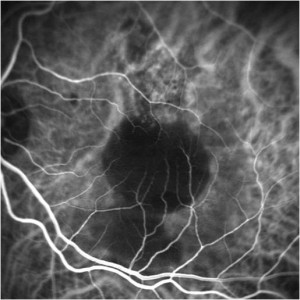
FAG, ICGA and OCT
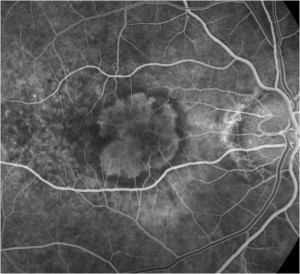
Three techniques are currently used to diagnose AMD imaging:
1) Retinal fluorangiography (FAG - Fluorescein Angiography)
2) Angiography with Indocyanine Green (ICGA - Indocyanine Green Angiography)
3) Optical Tomography with Coherent Light (OCT - Optical Coherence Tomography)
These are examinations with different and complementary properties.
FAG and ICGA are angiographic examinations that exploit the fluorescence principle of dyes, which are: fluorescein for FAG and indocyanine green for ICGA.
The FAG is ideal for examining the retina, while the IGCA is used to study the choroid; in both examinations, the images obtained are black and white and the presence of the dye (fluorescence) appears white.
- The FAG is the oldest eye test (1960s) and is still the gold standard in the assessment of macular lesions. In fact, once intravenously injected fluorescein reaches the retina, due to its physico-chemical properties, it cannot (under normal conditions) cross the inner blood-retinal barrier and remains inside the retinal capillaries, from which it only escapes (leakage) in the presence of pathological conditions that cause it to rupture.
The limitation of FAG is related to the impossibility of accurately detecting what occurs at the level of the thin vessels of the choriocapillaris, where free fluorescein (not bound to serum proteins) is able to diffuse into the extravascular spaces.
- L'ICGAintroduced in the 1970s and fully developed in the 1990s, uses indocyanine green as a dye which, unlike fluorescein, binds integrally to serum proteins and, therefore, remains confined, under normal conditions, to the lumen of the choriocapillary vessels, which are impermeable to these proteins. Because of all its properties, the ICGA represents the ideal examination for studying the choroidal circulation and, therefore, for detecting the pattern of neovases in exudative AMD. Moreover, it is the only diagnostic means that allows the differentiation of different subtypes of vascular abnormalities (CNV, RAP and PCV) with certainty, but also to exclude their presence, such as in drusenoid and serous retinal pigmented epithelium (DEP) detachments.
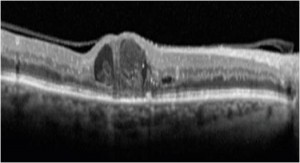
- L'OCT (Optical Coherence Tomography) is a recent technique that makes it possible to assess in vivo quantitative and qualitative changes in the macular region and optic nerve.
Introduced in 1991, OCT measures the reflection of light from the examined layers of the eye and has been validated for the diagnosis of macular diseases and in the glaucoma. The images acquired are high resolution and recently the Spectral Domain OCT, SDOCT, which has a higher image acquisition speed and theEDI-OCT, Enhanced Depth Imaging OCT, which also allows the study of the choroid.
Electrophysiological examinations
This is a series of examinations based on the detection of bioelectric signals emitted by the eyes and visual cortex in response to light stimuli to which they are subjected.
These tests provide a objective measure of the visual function and are very important, especially in the case of subjects who due to age (e.g. young children) or for other reasons (e.g. coma) are unable to give verbal responses or when there are significant opacities of the ocular dioptric media (cornea, crystalline lens, vitreous body).
The most commonly used electrophysiological examinations are:
a) Electroretinogram (ERG)
An ophthalmic test used to assess the functionality of the outer layers of the retina by means of a tracing, which records the changes in electrical potential of the retinal photoreceptors (cones and rods) in response to light flashes. It is carried out by applying electrodes near the eyes and on the cornea, which has previously been anaesthetised with special eye drops.
ERG can be useful in diagnosing retinal diseases such as retinal detachment, hereditary degeneration, retinal vasculopathies and is particularly important for the early diagnosis of retinitis pigmentosa.
b) Multifocal electroretinogram (mfERG)
This is the specific electrophysiological test for the macula, as it uses specially shaped light stimuli that evoke the response of only the photoreceptors and bipolar cells of this retinal district.
This test is of great importance for the early diagnosis of central retinal disorders, such as AMD, and for monitoring their course. In children, it is used to diagnose hereditary macular dystrophies, such as Stargardt's disease, and also makes it possible to detect ocular changes due to the side effects of certain medications.
c) Pattern electroretinogram (PERG)
It is used specifically to examine the ganglion cells of the macula, but actually allows the function of all layers of the macular retina to be assessed. In the PERG, stimuli are represented by a 'grid' (pattern), formed by black and white squares that change colour during the examination, all at the same time.
PERG can detect all diseases of the macula and is the most sensitive ophthalmic test for the early diagnosis of retinal degeneration, as well as for the assessment of macular involvement in the presence of retinitis pigmentosa. It can also be very useful for assessing ganglion cell function in the presence of glaucoma.
d) Visual evoked potentials (VEPs)
This eye test is used to assess the functioning of the visual nerve pathways from the retinal ganglion cells to the visual cerebral cortex. For this eye test, electrodes are applied to the forehead and the back of the skull, at the visual cortex. The stimulus used is normally a chessboard, which appears on a monitor, alternating light and dark (pattern reversal). For comatose or uncooperative patients, or children, a white light flash can be used. VEPs are used for the diagnosis of optic nerve dystrophies, demyelinating diseases (such as retrobulbar optic neuritis), and hereditary macular changes, such as macular dystrophies or cone and rod dystrophies. They are also used to diagnose side effects of certain drugs or in monitoring therapy in brain tumours.
Testing of dark adaptation (adaptorometry)
Assesses the eye's ability to adapt to low light conditions. This eye test is specific for the diagnosis ofhemeralopiacondition characterised by good day vision and poor night vision.
Autofluorescence measurement
The measurement of autofluorescence by retinography (fundus photography) is a recent eye test that is used to visualise the natural fluorescence of retinal pigment epithelium (EPR) cells under the effect of a certain illumination. The detection of autofluorescence takes only a few minutes and is useful in diagnosing EPR changes early, even before they are visible on slit-lamp examination of the eye fundus.
Dr. Carmelo Chines
Direttore responsabile