Phaco-trabeculectomy' is a combined surgical approach essentially reserved for glaucoma and cataract patients
A combined operation is defined as the performance of a simultaneous double surgical act to treat the concomitant presence of several pathologies. In the case of glaucoma, a combined surgical approach is essentially reserved for patients suffering from glaucoma and cataracts. At present, this surgical approach is being adopted more and more frequently in connection with both a considerable evolution in surgical techniques and an increase in the simultaneous presence of the two afflictions.
The first combined intervention of glaucoma and cataracts was proposed by Eustace1who performed an intracapsular technique without IOL implantation combined with trabeculectomy. Since then, there has been a considerable development of this procedure, the improvements of which can be attributed to the remarkable evolution of cataract and glaucoma surgical techniques2,3,4,5. In fact, the advent of phacoemulsification, foldable intraocular lenses inserted through mini-incisions, in conjunction with the development of trabeculectomy, antimetabolites and 'non-penetrating surgical techniques' (deep sclerectomy and viscocanalostomy) have appreciably improved the functional success of combined surgeries, reducing their complications6,7,8.
The association between glaucoma and cataracts is becoming increasingly common due to the increasing average age of life, as well as the prolonged tension compensation brought about by the latest drugs and antiglaucomatosis treatmentswhich has the effect of delaying surgical therapy9. The above data is supported by the studies carried out by Kini10 and highlighted in Table 1: the latter, in fact, clearly shows how the incidence rate of glaucoma and cataracts progressively increases with age, reaching 7.2% of glaucoma and 46.1% of cataracts in the oldest age group, between 75 and 85.
Another reason for the increased use of combined surgery is the fact that glaucoma surgery is known to induce the development of cataractespecially in those patients who already have a varying degree of opacification of the crystalline lens11,12. In a study by Lichter13 there is an increased incidence of cataracts not only in patients undergoing glaucoma surgery, but also in those undergoing medical therapy, regardless of the type of drug used: this could be related to the aqueous humour dynamics and the hypotonising effect of the drugs14. This circumstance may make it advantageous to perform combined surgery in those patients who have an initial cataract and have to undergo glaucoma surgery.
As a result of the above, over the last fifteen years an increasing number of surgeons, relying on the proven safety and efficacy of the phacoemulsificationon the one hand, and in the relative safety of anti-glaucomatous techniques on the other, has increasingly and early performed combined cataract and glaucoma surgeries in order to reduce the trauma induced by two separate surgical procedures.
There are many types of combined glaucoma and cataract surgery, with phacoemulsification being combined with various glaucoma surgery techniques15. However, given that in clinical practice the most commonly performed method is phacoemulsification combined with trabeculectomy (with or without antimetabolites), the present discussion will focus exclusively on the analysis of this surgical procedure.
In the case of simultaneous glaucoma and cataracts, it is logical to consider proceeding with combined surgery: the latter, in fact, helps reduce surgical trauma and speed up visual and functional recovery.
However, the decision to undertake such an intervention is always very complex and conditioned by multiple factors that can be briefly exemplified as follows16:
- the type of patient (age, compliance, personal needs, risk factors for glaucoma);
- the type of glaucoma;
- the state of the papilla of the optic nerve and the field of view (severity of glaucomatous damage);
- the pressure 'target' achieved and the type and number of drugs used;
- the desired pressure 'target' (to be assessed on a case-by-case basis);
- the degree of opacification of the crystalline lens;
- the safety of the planned surgery (high for phacoemulsification, fairly high for trabeculectomy);
- the effectiveness of the planned surgery (visual recovery and achievement of the pressure 'target').
Given the multiplicity of elements that may influence the assessment of whether or not to proceed with a combined operation and, subsequently, the choice of the method to be performed, it is extremely difficult to provide a general outline to assist in a decision that should therefore be made on a case-by-case basis17.
The latter can be conducted via two separate surgical accesses (two ways) or a single access (one way).
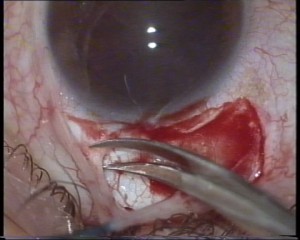
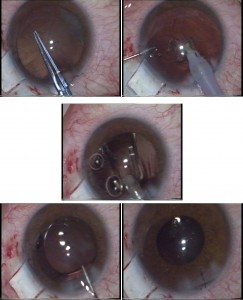
- execution, in the temporal sector with 'clear cornea' incision, of the various stages of phacoemulsification surgery with IOL implantation (Fig. 3 a-b-c-d-e);
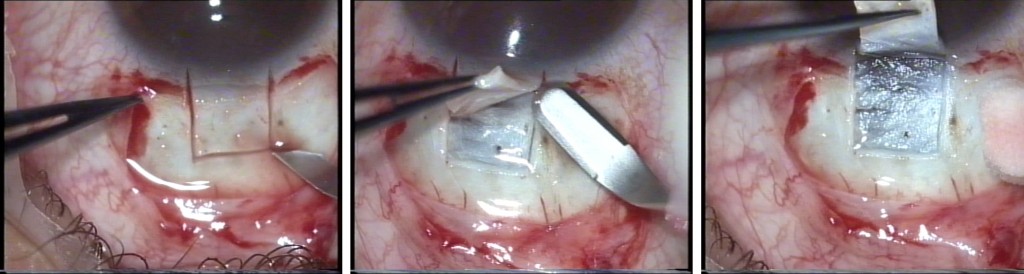
- removal of a plug of sclero-corneal tissue below the previously created scleral flap (Fig. 4 a-b); - performance of basal iridectomy with miosis pupil (created by the previous introduction of acetylcholine into the anterior chamber) (Fig. 5);
- Viscoelastic removal and suturing of the scleral flap with 2 or more 10/0 nylon stitches (Fig. 6 a-b);
- suture of the conjunctiva with vicryl 8/0 (Fig. 7).
- incision of the scleral tunnel from one or both sides to convert it into a flap (Fig. 11); some surgeons do not perform this stage of the operation and carry out the subsequent surgical time of removal of the sclero-corneal plug using an awl under the roof of the scleral tunnel, thus creating a 'stitchless phacotrabeculectomy';
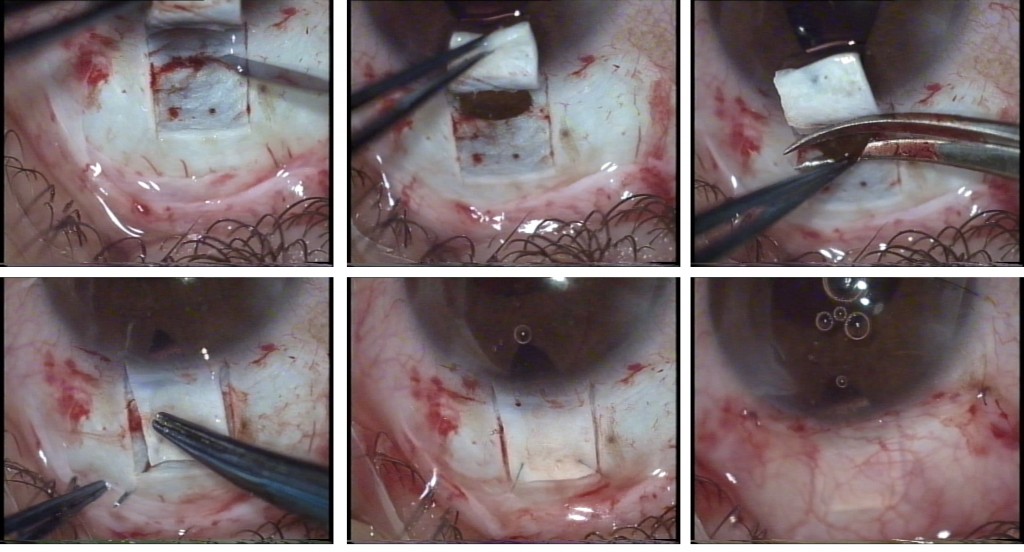
- removal of a plug of sclero-corneal tissue below the previously created scleral flap (Fig. 12 a-b).
- performing basal iridectomy with pupil in miosis (created by the previous introduction of acetylcholine into the anterior chamber) (Fig. 13);
- Viscoelastic removal and suturing of the scleral flap with 1 or more 10/0 nylon stitches (Fig. 14);
- suture of the conjunctiva with vicryl 8/0.
Results
Numerous studies in the literature have highlighted the beneficial effects associated with phacotrabeculectomy in terms of a significant reduction in the intraocular pressureregardless of what the initial IOP was. In particular18, highlighted the greater long-term effectiveness (2-year follow-up) of the trabeculectomy-facoemulsification combination compared to trabulectomy-extracpsular cataract extraction.
On the other hand, there is no agreement in the literature with regard to the functional results of phacotrabeculectomy compared to trabeculectomy and cataract surgery performed at different times, making it difficult to say which of the two procedures is the better one. In fact, some authors point out that the two methods present substantially similar outcomes in terms of intraocular pressure19,20.
In particular, el Sayyad21 compared phacotrabeculoctomy with mitomycin C trabeculectomy followed later by phacoemulsification surgery; the two groups had a similar IOP reduction, 14.6±3.7 mmHg for the combined procedure and 13.8±3.9 mmHg for the two-stage procedure. On the other hand, studies have shown a greater efficacy of trabeculectomy performed in isolation: in this regard, Kleinmann22 pointed out that trabulectomy with mitomycin C alone reduces intraocular pressure by 58.5%; whereas, phacotrabeculectomy with mitomycin C by 31.5%. The author, however, does not adequately elucidate the causes of these differences, which could be found in a greater trauma of combined surgery, which is followed by a superior alteration of the blood-water barrier or an increase in TGF-b (Transforming Growth Factor-beta)17,23.
Another highly controversial topic concerns the results of the two-way and one-way surgical technique, with regard to the greater effectiveness of one or the other. Numerous studies have shown a better result associated with performing the two-way technique both with regard to the reduction of the PIOthan to the number of drugs to be administered in the post-surgical period: this is due to the fact that less trauma is caused at the site of the trabeculectomy24,18,25,26. The two-way phacotrabulectomy is the method of choice for many surgeons, both for the reasons outlined above and because it is more suitable for performing a limbus-based conjunctival flap that does not hinder the performance of phacoemulsification.
A further highly debated issue is that of the alternative between the execution of a fornix-based or limbus-based conjunctival flap. Numerous studies on patients undergoing phacotrabulectomy have shown no major differences between the two methods with regard to both intraocular pressure and visual acuity27,28,29. However, when using antimetabolites, some surgeons prefer to perform a limbus-based flap in order to reduce filter draft 'leakage' in the immediate post-operative period30.
Finally, it should be emphasised that even for combined surgery there has been an increasing use of antimetabolites (5-fluorouracil and mitomycin C) in the last decade, with the aim of limiting cell proliferation and thus subconjunctival scarring. The literature on the subject has shown conflicting results on the efficacy of the use of these drugs in phacotrabulectomy. In particular, in a prospective randomised controlled trial it was found that phacotrabulectomy with 5-fluorouracil (5-FU) reduced intraocular pressure more than the same operation without the use of the antimetabolite31. In contrast, other studies have shown that the use of 5-FU does not lead to a significant improvement in functional results associated with combined surgery.25,32,33.
With regard to mitomycin C, numerous studies have shown that its use in phacotrabeculectomy improves pressor outcomes. In particular, in a double-blind controlled study by Cohen3performed on 72 patients who underwent phacotrabeculectomy with or without mitomycin C, 12 months after surgery, the group treated with the antimetabolite had a significantly lower IOP and required significantly fewer drugs than the control group. Similar results were found by Carlson34 in a study of 29 patients with a follow-up of 20 months. Jampel25in a meta-analysis of the literature published from 1964 to 2000, concluded that the use of mitomycin C and not that of 5-fluorouracil improves the results of phacotrabeculectomy in terms of intraocular pressure reduction. Finally, it should be emphasised that the use of mitomycin C is indicated in cases where the risk of filter failure appears greater or when a very low pressure 'target' has to be reached35.
In conclusion, phacotrabulectomy currently represents the elective intervention to treat the concomitant presence of glaucoma and cataract, in particular, in cases where a low pressure target has to be reached or the risk of failure of glaucoma surgery is high or, again, there is a very long life expectancy of the patient. Furthermore, according to the literature, the two-way technique with a fornix- or limbus-based conjunctival flap (the latter to be preferred when using antimetabolites) and the use of mitomycin C, rather than 5-fluorouracil, seem to be the most effective methods.
Complications combined glaucoma and cataract surgery
Complications of phacotrabeculectomy can arise from cataract surgery on the one hand and trabeculectomy on the other.
In the former case, ruptures of the posterior capsule or zonule could occur with possible loss of vitreous, damage endothelial, hypohaematous and expulsive haemorrhagesin the second case, hypotonos, atalamia, hypertone, anterior chamber fibrin, hypohaematous, haemovitreous, choroid detachment. Table 2 shows the incidence of the most common complications following phacotrabeculectomy, according to the data reported by the authors below.
Table, 2: Most common postoperative complications of phacotrabeculectomy
|
Author
|
Hypoema
|
Hypertone
|
Fibrin
|
Choroid detachment
|
|
Mamalis36
|
28%
|
5%
|
1%
|
3%
|
|
Anand37
|
28%
|
21%
|
12%
|
–
|
|
Perasalo38
|
16%
|
9%
|
18%
|
19%
|
|
Anders39
|
4%
|
–
|
–
|
–
|
|
Quentin40
|
–
|
–
|
10%
|
20%
|
|
Botz19
|
5%
|
–
|
6%
|
3.3%
|
As is clear from the above table, one of the most frequent complications, caused either by bleeding of the chamber angle or an episcleral vessel, or by irido-ciliary damage during trabeculectomy, is hypohaemas: the latter may be minor and, in such a case, usually tends to reabsorb quickly; but it may also be very extensive and, in such a case, washing of the anterior chamber may be indicated.
Turning to other complications, theocular hypertension in the immediate post-operative period is strictly dependent on how the scleral flap is closed and can often be easily resolved by the removal of one or more stitches from the flap itself.
The presence of fibrin in the anterior chamber, also a fairly frequent complication, appears to be related to the uveal reaction following surgery, and even in this case, a fairly quick remedy is the instillation of mydriatics.
As far as choroid detachment is concerned, which is certainly one of the most important complications of glaucoma surgery, its incidence rate varies greatly among the various authors, which suggests that it depends very much on the type of surgical technique used.
Furthermore, it must be remembered that one of the factors leading to a higher incidence of complications is the use of antimetabolites in combined surgery (as well as in trabeculectomy performed alone). In such a case, the complications that most frequently occur are corneal epitheliopathy (5-FU), aqueous leakage from the wound or the draft, hypotonia, draft inflammation and endophthalmitis41.
In a study by Kuroda42 comparing phacotrabeculectomy and trabeculectomy alone, both using mitomycin C, the former method was found to have fewer postoperative complications than the latter.
In conclusion, in view of the above, it can be stated that the combination of trabeculectomy (with or without antimetabolites) combined with phacoemulsification not only represents a relatively safe surgical technique, but does not have a higher incidence of complications than trabeculectomy performed alone.
Conclusions
The simultaneous presence of glaucoma and cataract is an increasingly common phenomenon due to both the increase in the average age of life and the prolonged tension compensation that is induced by the latest glaucoma drugs and treatments and on which the delay in surgical therapy depends. For these reasons, very often the surgeon who has to deal with these two diseases is faced with the choice of performing two separate operations or proceeding with a combined operation.
In particular, the surgical options that can be implemented in the presence of cataracts and glaucoma are: 1) glaucoma surgery and subsequent phacoemulsification;
2) phacoemulsification and subsequent glaucoma surgery;
3) combined intervention15.
Precisely with reference to the surgeon's choice between the above-mentioned methods, some authors have, however, pointed out that the functional result of trabeculectomy risks being adversely affected by the subsequent phacoemulsification operation due to the slight intraocular inflammation that the latter causes43,44.
In light of these considerations, the most advantageous options for the surgeon are, therefore, phacoemulsification and subsequent glaucoma surgery or combined surgery. In this regard, since the literature does not offer certain data regarding the greater functional efficacy of one or the other method, the choice between them is complex and in fact entrusted to the surgeon's experience and to the evaluation of numerous factors such as, for example, the basal pressure value, the number of drugs used, the pressure target to be reached, the severity of the glaucomatous damage and the extent of the cataract.
Recently, more and more surgeons are deciding to address the coexistence of glaucoma and cataract through the combined surgeryThis decision is, moreover, encouraged by the increasing sophistication of glaucoma and cataract surgical techniques. On the other hand, confirming the validity of the choice of a combined operation, multiple studies have highlighted its considerable functional effectiveness, as well as its safety especially in terms of complications.
As for the technique to be used for performing the phacotrabeculectomy, the one to be preferred is the two-way technique with a fornix- or limbus-based conjunctival flap (the latter to be preferred when using antimetabolites)45. Moreover, with reference to antimetabolites, their use is more indicated in cases where the risk of filtration failure is higher or a very low target pressure needs to be reached: in particular, the use of mitomycin C has been indicated as preferable to 5-fluorouracil for this purpose.
Antonio Marino, Daniela Rita Lombardo, Lorenzo Rapisarda
The Authors: Antonio Marino, Daniela Rita Lombardo belong to the Complex Operative Unit of Ophthalmology of the Azienda Ospedaliera di Rilievo e di Alta Specialità Garibaldi of Catania, while Dr. Lorenzo Rapisarda belongs to the Complex Operative Unit of Ophthalmology of the Umberto I Hospital of Syracuse Asp N. 8.
Their scientific, clinical and surgical activity is marked by a particular interest in glaucomatous disease.
Bibliography
1. Eustace P, Harun AQ. Trabeculectomy combined with cataract extraction. Trans Ophthalmol Soc UK. 1974; 94: 1058-1063.
2. Allan BD, Barrett GD. Combined small incision phacoemulsification and trabeculectomy. J Cataract Refract Surg. 1993; 19: 97-102.
3. Cohen JS, Greff LJ, Novack GD, Wind BE. A placebo-controlled, double-masked evaluation of mitomycin C in combined glaucoma and cataract procedures. Ophthalmology. 1996; 103: 1934-1942.
4. Jay JL. Extracapsular lens extraction and posterior chamber intraocular lens insertion combined with trabeculectomy. Br J Ophthalmol. 1985; 69: 487-490.
5. McCartney DL, Memmen JE, Stark WJ, et al. The efficacy and safety of combined trabeculectomy, cataract extraction and intraocular lens implantation. Ophthalmology. 1988; 95: 754-763.
6. el Sayyad FF, el Maghraby MA. The contribution of phacoemulsification to combined cataract and glaucoma surgery. Curr Opin Ophthalmol. 1998; 9: 95-100.
7. Gianoli F, Schnyder CC, Bovey E, Mermoud A. Combined surgery for cataract and glaucoma: phacoemulsification and deep sclerectomy compared with phacoemulsification and trabeculectomy. J Cataract Refract Surg. 1999; 25: 298-300.
8. Samuelson TW. Surgical management of coincident cataract and glaucoma. Curr Opin Ophthalmol. 1997; 8: 39-45.
9. Raiita C, Tarkkanen A. Combined procedure for the management of glaucoma and cataract. Acta Ophthalmol 1988; 66: 667-670.
10. Kini MM, Leibowitz HM, Colton T, et al. Prevalence of senile cataract, diabetic retinopathy, senile macular degeneration, and open-angle glaucoma in the Framingham eye study. Am J Ophthalmol. 1978; 85: 28-34.
11. AGIS Investigators. The Advanced Glaucoma Intervention Study: Risk of cataract formation after trabeculectomy: Arch Ophthalmol. 2001; 119: 1771-1779.
12. Hylton C, Congdon N, Friedman D, et al: Cataract after filtration surgery: Am J Ophthalmol. 2003; 135: 231-232.
13. Lichter PR, Musch DC, Gillespie BW, et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001; 108: 1943-1953.
14. Lee RK, Gedde SJ. Surgical management of coexisting cataract and glaucoma. Int Ophthalmol Clin. 2004; 44: 151-166.
15. Verges C, Cazal J, Lavin C. Surgical strategies in patients with cataract and glaucoma. Curr Opin Ophthalmol. 2005; 16: 44-52.
16. Bellucci R. Cataract and glaucoma. In Cataract SOI report. Fabiano Publisher. 1999; 447-473.
17. Vass C, Menapace R. Surgical strategies in patients with combined cataract and glaucoma. Curr Opin Ophthalmol. 2004; 15: 61-66.
18. Friedman DS, Jampel HD, Lubomski LH, et al. Surgical strategies for coexisting glaucoma and cataract: an evidence-based update. Ophthalmology. 2002; 109: 1902-1913.
19. Botz N, Heider W. Long-term influence of pre-, intra-, and postoperative factors on the intraocular pressure in combined cataract and glaucoma surgery. Ophthalmologe. 2004; 101: 1202-1208.
20. Donoso R, Rodriguez A. Combined versus sequential phacotrabeculectomy with intraoperative 5-fluorouracil. J Cataract Refract Surg. 2000; 26: 71-74.
21. el Sayyad FF, Helal MH, Kalil MM, el Maghraby MA. Phacotrabeculectomy versus two-stage operation: a matched study. Ophthalmic Surg Lasers. 1999; 30: 260-265.
22. Kleinmann G, Katz H, Pollack A, et al. Comparison of trabeculectomy with mitomycin C with or without phacoemulsification and lens implantation. Ophthalmic Surg Lasers. 2002; 33: 102-108.
23. Siriwardena D, Kotecha A, Minassian D, et al. Anterior chamber flare after trabeculectomy and after phacoemulsification. Br J Ophthalmol. 2000; 84: 1056-1057.
24. el Sayyad FF, Helal MH, el Maghraby MA, et al. One-site versus two-site phacotrabeculectomy: a randomised study. J Catract Refract Surg. 1999; 25: 77-82.
25. Jampal HD, Friedman DS, Lubomski LH, Kempen JH, et al. Effect of technique on intraocular pressure after combined cataract and glaucoma surgery: an evidence-based review. Ophthalmology. 2002; 109: 2215-2224.
26. Wyse T, Meyer M, Ruderman JM, et al. Combined trabeculectomy and phacoemulsification: One-site vs two-site approach. Am J Ophthalmol. 1998; 125: 334-339.
27. Berestka JS, Brown SVL. Limbus versus fornix-based conjunctival flaps in combined phacoemulsification and mitomycin C trabeculectomy surgery. Ophthalmology. 1997; 104: 187-196.
28. Shingleton BJ, Chaudhry IM, O'Donoghue MW, et al. Phacotrabeculectomy: limbus-based versus fornix-based conjunctival flaps in fellow eyes. Ophthalmology. 1999; 106: 1152-1155.
29. Tezel G, Kolker AE, Kass MA, et al. Comparative results od combined procedures for glaucoma and cataract: II: limbus-based versus fornix-based conjunctival flaps. Ophthalmic Surg Lasers. 1997; 28: 551-557.
30. Kozobolis VP, Siganos CS, Christodoulakis EV, et al. Two-site phacotrabeculectomy with intraoperative mitomycin-C: fornix- versus limbus-based conjunctival opening in fellow eyes. J Cataract Refract Surg. 2002; 28: 1758-1762.
31. Gandolfi SA, Vecchi M. 5-Fluoruracil in combined trabeculectomy and clear cornea phacoemulsification with posterior chamber intraocular lens implantation. Ophthalmology. 1997; 104: 181-186.
32. Cohen JS. Combined cataract implant and filtering surgery with 5-fluorouracil. Ophthalmic Surg. 1990; 21: 181-186.
33. Wong PC, Ruderman JM, Krupin T. 5-Fluorouracil after primary combined filtration surgery. Am J Ophthalmol. 1994; 117: 149-154.
34. Carlson DW, Alward WLM, Barad JP, et al. A randomised study of Mitomycin augmentation in combined phacoemulsification and trabeculectomy. Ophthalmology. 1997; 104: 719-724.
35. Shin DH, Ren J, Juzych MS, et al. Primary glaucoma triple procedure in patients with primary open-angle glaucoma: the effects of mitomycin C in patients with and without prognostic factors for filtration failure. Am J Ophthalmol. 1998; 125: 346-352.
36. Mamalis N, Lohner S, Rand AN, Crandall AS. Combined phacoemulsification intraocular lens implantation and trabeculectomy. J Cataract Refract Surg. 1996; 22: 467-473.
37. Anand N, Menage MJ, Bailey C. Phacoemulsification trabeculectomy compared to other methods of combine cataract and glaucoma surgery. Acta Ophthalmol Scand. 1997; 75: 705-710.
38. Perasalo R, Flink T, Lehtosalo J, et al. Surgical outcome of phacoemulsification combined with trabeculectomy in 243 eyes. Acta Ophthalmol Scand. 1997; 75: 581-583.
39. Anders N, Pham T, Holschbach A, Wollensak J. Combined phacoemulsification and filtering surgery with the "no-stitch" technique. Arch Ophthalmol. 1997; 115: 1245-1249.
40. Quentin CD, Dittmer K, Lauritzen L, et al. Combined glaucoma and cataract operation with fondable posterior chamber lens implantation. Long-term outcome and complications. Ophthalmologe. 2000; 97: 753-757.
41. Lama PJ, Fechtner RD. Antifibrotics and wound healing in glaucoma surgery. Surv Ophthalmol. 2003; 48 :314-346.
42. Kuroda S, Mizoguchi T, Terauchi H, Nagata M. Trabeculectomy combined with phacoemulsification and intraocular lens implantation. Semin Ophthalmol. 2001; 16: 168-171.
43. Derbolab A, Vass C, Menapace R, et al. Long-term effect of phacoemulsification on intraocular pressure after trabeculectomy. J Cataract Refract Surg. 2002; 28: 425-430.
44. Park HJ, KwonYH,, Weitzman M, et al. Temporal corneal phacoemulsification in patients with filtered glaucoma. Arch Ophthalmol.1997; 115: 1375-1380.
45. Liu NH, Chen XL, Li X, et al. Efficacy and tolerability of one-site versus two-site phacotrabeculectomy: a meta-analysis of randomised controlled clinical trials. Chin Med J. 2010; 123 (15): 2111-115.
Dr. Carmelo Chines
Direttore responsabile