Introduction
The use of hyaluronic acid filler to carry out aesthetic procedures in the periocular area is now a very popular and sought-after procedure, since it is considered a minimally invasive ophthalmoplastic procedure that provides rapid and - not least - pain-free aesthetic benefits.
Hyaluronic acid
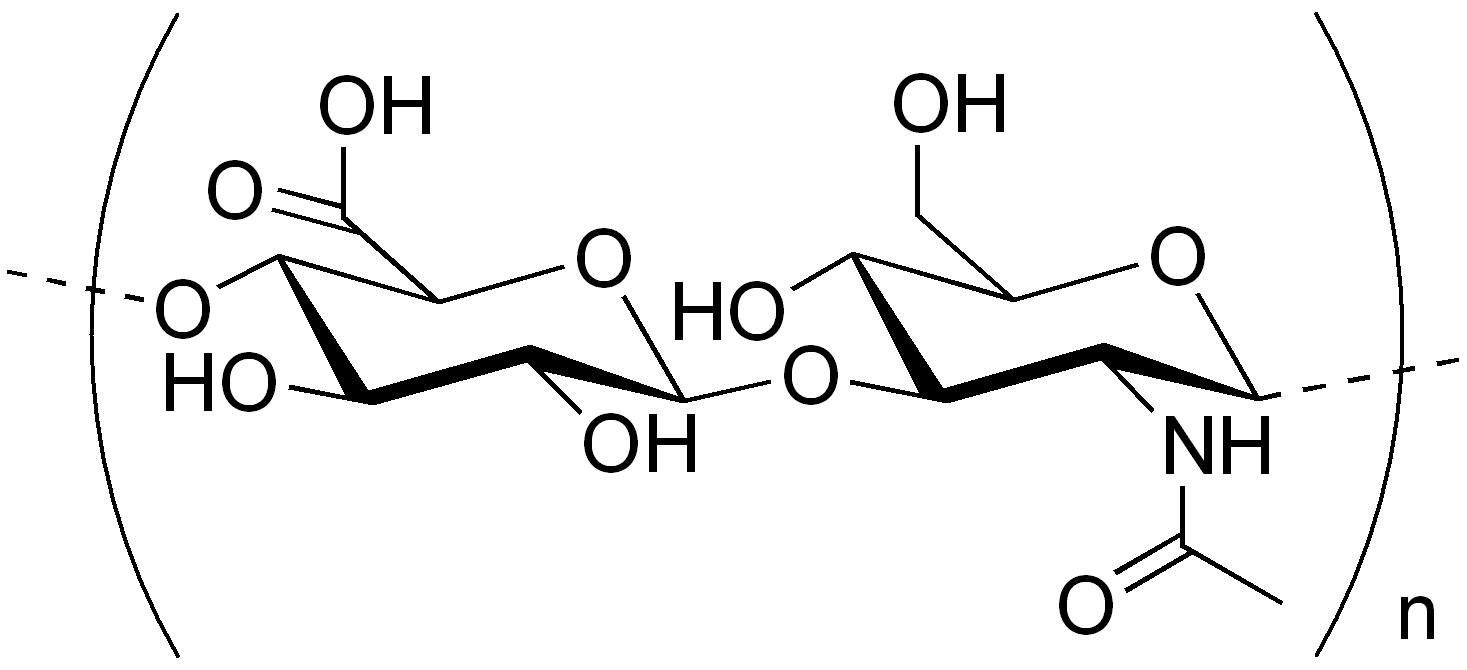
L'hyaluronic acid is a high molecular weight polyanionic polysaccharide with a typical spiral structure that gives it a particular ability to combine with water1 and an excellent viscoelasticity.
This results in an excellent moisturising capacity and a pronounced pseudoplastic behavioursimilar to that of the soluble mucins in the tear film.
What pseudoplastic means
In fluid mechanics, 'pseudoplastic' is said of non-Newtonian fluids in which the coefficient of viscosity decreases as shear stress increases.
In the case of hyaluronic acid contained in eye drops, 'pseudoplastic' means that it has a higher viscosity when the eye is open and a lower viscosity during blinking, allowing lubrication of the entire ocular surface.
Properties
The properties Hyaluronic acid's ability to bind large amounts of water and its ability to mimic the behaviour of mucins help maintain the stability of the tear film and ensure optimal protection and lubrication of the eye.
In addition to possessing these special properties, hyaluronic acid also plays an important biological role in the processes of corneal repair promoting cell motility, adhesion and proliferation.
L'hyaluronic acid is a high molecular weight polyanionic polysaccharide with a typical spiral structure that gives it a particular ability to combine with water1 and an excellent viscoelasticity.
This results in an excellent moisturising capacity and a pronounced pseudoplastic behavioursimilar to that of the soluble mucins in the tear film.
What pseudoplastic means
In fluid mechanics, 'pseudoplastic' is said of non-Newtonian fluids in which the coefficient of viscosity decreases as shear stress increases.
In the case of hyaluronic acid contained in eye drops, 'pseudoplastic' means that it has a higher viscosity when the eye is open and a lower viscosity during blinking, allowing lubrication of the entire ocular surface.
Properties
The properties Hyaluronic acid's ability to bind large amounts of water and its ability to mimic the behaviour of mucins help maintain the stability of the tear film and ensure optimal protection and lubrication of the eye.
In addition to possessing these special properties, hyaluronic acid also plays an important biological role in the processes of corneal repairpromoting cell motility, adhesion and proliferation.
The risks of fillers
Intervening on the periocular area carries certain risks, not least because of the changes that ageing brings about in the orbicularis muscles, malar and post-septal adipose tissue, the orbital septum and ligaments such as the zygomatic-cutaneous ligament and the orbicularis ligament.
The effects of ageing
Due to ageing, the elasticity of the skin under the eyes decreases, fat and muscles atrophy and herniation occurs due to weakening of the orbital septum and ligaments.
Reduced muscle support and redistribution of adipose tissue promote oedemas and malar accumulations under the eyes, which contribute to a puffy face that is among the causes of people's dissatisfaction with their appearance and prompts them to resort to aesthetic treatments.
Possible complications
In these cases, improper or excessive use of fillers can lead to complications, such as filler migration, i.e. its spread to an area other than the injection site, and the formation of a foreign-body granuloma.
Durability over time
Recent studies have shown that fillers based on hyaluronic acid can persist for years, compared to the previously assumed duration of 3-12 months, with the risk that too frequent injections can lead to unwanted swelling and the formation of granulomas.
Filler-induced injuries
These lesions are the result of an inflammatory response to the injected material and are caused by macrophages fusing into giant multinucleated cells.
Injecting hyaluronic acid fillers into the wrong area or periocular plane can also lead to the same complications.
Type of injury
The set of changes induced by hyaluronic acid injection treatment include:
- sunken facial tissue
- oedemas
- visible nodules
- Tyndall effect
The Tyndall effect is a bluish discolouration of the skin caused by light scattering and occurs when hyaluronic acid is injected too superficially.
Intramuscular injection of HA can, on the other hand, lead to mobility problems, altering natural periocular movement.
Prerequisites for injection therapy
Well-established experience in injection therapy and a thorough knowledge of ocular anatomy are, therefore, crucial.
Strict patient selection must also be carried out, treating only individuals with good skin elasticity and mild to moderate volume loss.
These types of patients generally achieve the best results compared to those with more than 1 cm of excess skin.
Pre-treatment imaging
Imaging techniques are very useful to visualise the soft tissues and the vascular network feeding them, to monitor filler placement and, if necessary, to manage any complications.
In particular, computerised magnetic resonance imaging (MRI) can be useful for this purpose.
How to manage filler complications
To combat complications due to migrated fillers, one must first reconstruct the patient's medical history and acquire information on the type and volume of substance which was injected.
At this point, a specific solvent, to be handled with extreme caution, is used, the hyaluronidase, which is a toxin whose action is similar to the effect of phospholipases.
Hyaluronidase
Hyaluronoglucosaminidases or hyaluronidases are enzymes belonging to the class of hydrolases that degrade hyaluronic acid by hydrolysing its 1→4 bonds between N-acetyl-β-D-glucosamine and D-glucuronate residues.
They are also capable of hydrolysing the 1,4-β-D-glycosidic bonds between N-acetylgalactosamine or N-acetylgalactosamine sulphate and glucuronate in chondroitin between N-acetylgalactosamine sulphate and glucuronic acid in chondroitin, chondroitin 4-sulphate and 6-sulphate and in dermatan.
By catalysing the hydrolysis of hyaluronic acid, which is a major constituent of the intestinal barrier, hyaluronidase lowers the viscosity of the acid, increasing tissue permeability.
Hyaluronidase resists drying and ageing well.
It is used in medicine together with other drugs to facilitate their spread. One of the most common examples is in ophthalmic surgery, where they are used with local anaesthetics.
It may possibly be used after consulting pharmacological texts and treatises to avoid interactions with the chemotherapeutic agent and duly diluted in the treatment of the latter.
Some bacteria, such as Staphylococcus aureus, Streptococcus pyogenes, or Clostridium perfringens, produce hyaluronidase in order to have greater mobility through the tissues of the human body and this allows it to be unrecognised by the macrophages of our immune system.
In the globulin fraction of blood, there are elements (which are not antibodies), such as 'Haas anti-invasins', capable of hindering tissue invasion by hyaluronidase-producing pathogens.
Treatment modes
There is currently no established protocol for the administration of hyaluronidase, which is an enzyme capable of degrading certain components of the extracellular matrix, such as hyaluronic acid.
The hyaluronidase acts by breaking the glycosidic bonds present in hyaluronic acid.
The 'posthyaluronidase syndrome'
Improper and incorrect use can lead to the so-called 'posthyaluronidase syndrome'.
It is a syndrome characterised by sagging and loss of volume of the facial tissue, depigmentation and loss of elasticity of the periocular skin.
This type of side effects can even lead to a worsening of the aesthetic situation that had been determined before the injection treatment and its complications.
About hyaluronic acid see also:
- Sodium hyaluronate and dry eye after cataract surgery - Oculista Italiano
- Hyaluronic acid and xanthan gum for the wellbeing of the ocular surface
- Hyaluronic acid in ophthalmology
- Wilde CL, Jiang K, Lee S, Ezra DG. The Posthyaluronidase Syndrome: Dosing Strategies for Hyaluronidase in the Dissolving of Facial Filler and Independent Predictors of Poor Outcomes. Plast Reconstr Surg Glob Open. 2024 Apr 23;12(4):e5765. doi: 10.1097/GOX.0000000000005765. PMID: 38655103; PMCID: PMC11037726.
- Master M, Azizeddin A, Master V. Hyaluronic acid filler longevity in the mid-face: a review of 33 magnetic resonance imaging studies. Plast Reconstr Surg Glob Open. 2024;12(7):e5934. doi:10.1097/GOX.0000000000005934
- Kim HJ, Kwon SB, Whang KU, et al. The duration of hyaluronidase and optimal timing of hyaluronic acid (HA) filler reinjection after hyaluronidase injection. J Cosmet Laser Ther. 2018;20:52-57.
