Those suffering from EMD know that among the most common symptoms and discomforts are a distorted vision and an impaired perception of colour vision, that can cause a extreme difficulty in performing daily activities, such as writing, reading or driving.
In these terms, the loss of central vision results in a significant reduction in quality of life and the ability to independently manage essential daily activitiesconditions that worsen considerably if EMD affects both eyes. It is not uncommon, in fact, for EMD sufferers to also complain of states depressive emotional which combine to a high risk of falls and accidents as a result of visual loss and how it all contributes the impairment of working capacity.
What are the treatment options for EMD?
To date, there are different therapeutic strategies capable of slowing down the course of EMD, also indicated by national guidelines.
Among the first-line treatments for the form of EMD that does not involve the centre of the retina is the laser photocoagulationa well-established technique in the management of the disease. However, this approach may be associated with side effects, such as the possibility of some scarring in the retinal area.
For the treatment of EMD affecting the macular area, however, the intravitreal drug administration, known as anti-VEGF agents (VEGF, vascular endothelial growth factor), capable of counteracting the massive production of vascular endothelial growth factor, and thus counteracting the growth of neovases and thus slowing down and improving the pathological condition. However, in this case, it is need to undergo a large number of annual intravitreal injections e of medical examinations.
For all those who cannot be treated with anti-VEGF drugs or who have not responded adequately to first-line treatmentsthe guidelines indicate the intravitreal administration of corticosteroids, including fluocinolone acetonide (FAc).
Diabetic macular oedema: causes and risk factors
L'diabetic macular oedema (EMD) is a of the most serious complications of diabetic retinopathy (RD), an ocular pathology that can occur in patients with diabetes, precisely because of the pathological disruption caused by hyperglycaemia. EDM is characterised by the disruption of the blood-retinal barrier, i.e. a 'protection' that under normal conditions prevents certain substances from entering the retinal tissue, and by an increase in vascular permeability that causes fluid and other plasma constituents to spill into or near the macula, the central portion of the retina that is the most sensitive to light stimuli and is responsible for distinct central vision.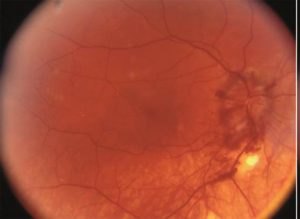
The causes of the onset of EMD can be of various kinds and include, inflammatory processes, angiogenetic processes (the formation of new blood vessels) and processes linked to oxidative stress phenomena, a condition caused by the excessive production of free radicals, i.e. molecules that are potentially harmful to our organism. Risk factors for the onset of EMD may include:
- l'hyperglycaemia, i.e. high blood glucose levels leading to the massive and uncontrolled production of several molecules including vascular endothelial growth factor (VEGF, vascular endothelial growth factor), responsible for the excessive production of new blood vessels and an increase in their permeability
-the duration of diabetesClinical evidence shows that the likelihood of EMD increases with the duration of diabetic disease.
For whom is AFc-based intravitreal implantation indicated and what benefits does it bring?
As of 2016, it is also available in Italy for patients who are insufficiently responsive to first-line treatments, a new intravitreal corticosteroid treatment, which guarantees a slow and prolonged release of fluocinolone acetonide (FAc) for a period total of three years. In terms of efficacy, this drug has been shown to improve the patient's visual acuity and the structural and functional status of the central portion of the macula.
These advantages translate into a better quality of life. Indeed, when not strictly adhering to the pharmacological regimen prescribed by the doctor, where it involves several annual intravitreal injections, one may face a reduction in therapeutic success and an increased likelihood of complications related to the same treatment modalities (possible infections, injection discomfort, frequent absences from work, etc.) . The implantation of AFc, on the other hand, is a very practical approach for all EMD sufferers as the availability of a single-dose drug with at least three years' coverage of action is an easier treatment regimen to follow.
The acquisition of lost visual capacityFinally, it allows the EMD patient to return to common daily activities and resume normal life rhythms without the need to depend on family members. The regaining of one's independence contributes significantly to a psychological well-being and to a more positive moodvital factors for all people suffering from chronic diseases.
Finally, what should be done to prevent or slow down the ocular complications of diabetes?
The person with diabetes, as indicated by the guidelines published in 2015 by the Italian Society of Diabetology (SID), in order to prevent and counteract the onset and progression of the disease, and reduce the possibility of experiencing irreversible complications, should:
-monitor blood glucose levels periodically
-undergo eye check-upswhich allow the presence of damage in the retinal vascular layer to be detected.
Bibliography:
-Guidelines for the screening, diagnosis and treatment of diabetic retinopathy in Italy, Working Group on Ocular Complications of Diabetes, Italian Society of Diabetology, 2015
-American Academy of Ophthalmology Retina/Vitreous Panel. Preferred Practice Pattern_ Diabetic retinopathy. 2016.
Dr. Carmelo Chines
Direttore responsabile
