Cataract surgery today has reached unprecedentedly high standards.
 The calculating precision of biometers, the use of topo-aberrometers, the use of Premium High-Technology lenses to correct astigmatism and presbyopia, and finally the advent of the Femtolaser, which further enhances the already excellent surgical performance of sophisticated phacoemulsifiers, make cataract removal a microsurgical procedure with high refractive expectations that, more often than not, succeeds in achieving the expected result.
The calculating precision of biometers, the use of topo-aberrometers, the use of Premium High-Technology lenses to correct astigmatism and presbyopia, and finally the advent of the Femtolaser, which further enhances the already excellent surgical performance of sophisticated phacoemulsifiers, make cataract removal a microsurgical procedure with high refractive expectations that, more often than not, succeeds in achieving the expected result.
Yet, very often, the post-surgery of perfect eyes already on the first day is punctuated by discomfort from patients who report foreign body sensation, tearing, burning and photophobia1.
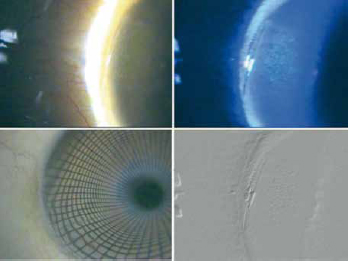
Unfortunately, the act of surgery with the ensuing inflammatory process, the use of powerful disinfectants in the pre- and post-operative period and the use of eye drops with preservatives2can easily lead to an alteration of the lachrymal film with the appearance of the whole parade of symptoms that turn a perfect surgical intervention into a failure for the patient. The execution of the incisions themselves is also responsible for the foreign body sensation that the patient sometimes reports with such insistence that he does not appreciate the functional recovery achieved (Fig. 1).
Post-operative dyslacrimia may have an acute course with short-lived manifestations and subsequently recur within a few weeks, or it may become chronic and have a longer lasting course.
Dry-eye symptoms in post-cataract surgery may involve patients already suffering from a pre-existing condition, with worsening of symptoms, and previously healthy patients with no evidence of symptoms prior to surgery.
What are then the elements responsible for the appearance of this symptomatology? Are there any modifiable predisposing factors? How can we prevent the onset of symptoms and reduce their duration?
Factors involved in the onset or exacerbation of symptoms include the incision site and its morphology, the duration of the operation, the pre-existence of dry-eye and the presence of any systemic pathologies such as diabetes, collagenopathies and other autoimmune pathologies co-responsible for altering the tear film.
A certain influence can also be attributed to the pre-operative procedure and the post-operative medical therapy, especially if it is carried out with preparations with aggressive preservatives such as Benzalkonium chloride.
A point of particular interest is the incision-induced impairment of the corneal innervation.
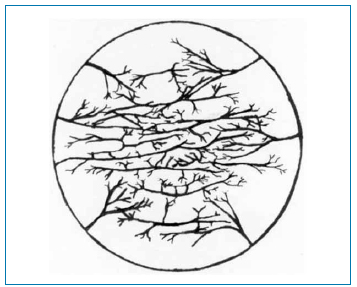
The long branches of the ciliary nerve (sensory innervation of the cornea) penetrate the limbus mainly at 3 o'clock and 9 o'clock (Fig. 2).
When damage to the corneal nerve endings occurs, it leads to increased epithelial permeability, reduced metabolic activity and an abnormal healing process. Corneal innervation plays a role in the repair processes of the corneal epithelium and also controls tear secretion.
For this reason, an attempt is made, whenever possible, not to make the incisions at 3 and 9 o'clock, but to move them a few degrees apart, thus avoiding severing many corneal nerve endings.
At the Clinica Mediterranea in Naples we are starting a comparison study on the side effects reported by patients operated on cataracts with the traditional technique compared to those operated with Femtocataract in order to compare the possible different effects of scalpel incisions compared to incisions made with our new Femtosecond laser (LenSxAlcon). It will certainly be interesting, considering the role that incisions play in the genesis of post-operative discomfort, to evaluate the effect of incisions made with the Femtosecond laser for cataracts on the onset and development of post-operative dyslacrimia.
In Femtocataract, since the incision is achieved by non-thermal photodestruction through a sequence of adjacent cavitation bubbles, less stromal inflammation is induced in the incision area.
But the incision, whatever the technique performed, is a surgical moment that cannot be avoided!
In the genesis of post-operative discomfort, there are other phases with procedures to be improved for patient comfort. Certainly, the pre-operative phase and intra- and post-operative management play a decisive role on the occurrence and duration of dyslacrimia.
Pre-operative preparation
The analysis of the patient undergoing cataract surgery is crucial for the prevention and management of dry-eye and dyslacrimia.
Particular attention should be paid to the quality and quantity of the tear film, the possible presence of dysfunction of the Meibomian glands (MGD), the possible presence of eyelid malocclusions, ongoing infectious processes and alterations of the tear ducts.
The presence of an altered tear film, even if not symptomatic, may be responsible for post-surgical discomfort due to the exacerbation of dyslacrimia with significant post-operative symptoms.
The possible presence of evaporative dry-eye from MGD and the concomitant presence of blepharitis must necessarily be treated before cataract surgery in order to reduce the inflammatory process and improve the quality of the tear film.
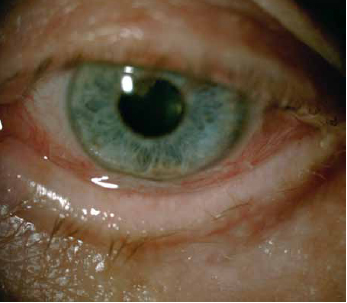
The presence of anatomical changes (irregularities of the eyelid margin, neovascularisation of the border, advancement of the grey line) (Fig. 3) are also indicative of chronic inflammatory processes that must necessarily be treated with the use of appropriate lubricants and often also low-dose cortisone for prolonged periods of time, in cycles of e.g. 5-10 days, to be repeated monthly.
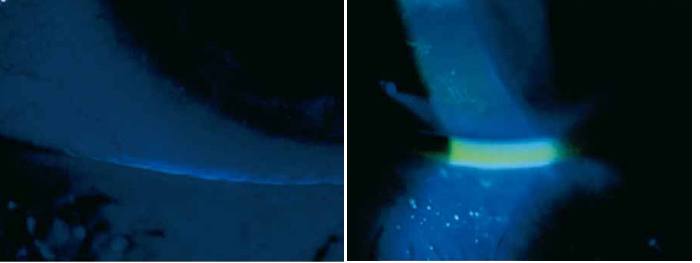
The identification of dry-eye, of which the patient must be made aware, and the appropriate preoperative therapy are decisive in the correct management of the cataract surgery subject and his expectations (Fig. 4).
In the preparation of the patient, excessive use of aggressive local anaesthetics, mydriatics with added phenylephrine and excessive dwell time of Iodopovidone at inadequate concentrations lead to damage to the conjunctival mucosa and calycephalic cells with consequent alteration of the pre-corneal tear film. All these substances also lead to a certain degree of toxicity of the delicate structures deputed to the removal of tears such as the mucosa of the lacrimal puncta, the sphincter and the first part of the lacrimal canaline with consequent difficult drainage of the tears themselves and epiphora.
Another extremely important aspect in preparing the patient for cataract surgery is the prevention of post-operative infections.
In accordance with international surgical protocols, to prevent endophthalmitis, it is good practice to instill antibiotic eye drops pre-operatively, possibly in a single-dose formulation, as it has been shown that in the majority of cases the pathogens responsible for post-operative endophthalmitis originate from the bacterial flora present on the patient's conjunctiva and periocular skin4.
The antibiotic used pre-operatively should be the same as that used post-operatively, possibly in a formulation combined with the corticosteroid and preferably always in a single dose to avoid epithelial damage from the preservative.
Intraoperative management
Intraoperative management of the surgical patient plays a role of great importance not only for the successful outcome of the surgery, but also and above all to avert the possible occurrence of post-operative discomfort, including the occurrence of the dreaded dry-eye.
Patient disinfection: The sterilisation procedure of the operating field is mandatory and of utmost importance for the prevention of post-operative infections. According to international protocols, the use of iodopovidone diluted to 5% for the conjunctival sac and 10% for cleaning the eyelids and periocular skin is indispensable5-7. A patient who has an ongoing conjunctival or lacrimal tract infection during surgery must necessarily be postponed and postponed until after healing.
It must be remembered that the use of iodopovidone, although indispensable for sterilising the surgical field, plays a highly aggressive role on the conjunctival mucosa, contributing to the development of discomfort evident in the post-operative period.
The use of dosages at lower concentrations of iodopovidone, however, have been shown not to be effective in preventing post-operative infections8.
The dilation and anaesthesia procedure must also follow strict rules to avoid the appearance and exacerbation of symptoms.
Furthermore, each patient must be characterised for his or her clinical condition. Patients with autoimmune diseases with ocular involvement, severe dry-eye or Sjögren's syndrome present a precarious corneo-conjunctival balance. The overuse of anaesthetics and mydriatics in this category of patients inevitably leads to the appearance of ocular discomfort in the post-operative period, up to actual manifestations of corneal dysepithelialisation with subsequent inflammation and pain.
Post-operative management
Post-operative management of the patient undergoing cataract surgery aims to reduce ocular inflammation, prevent the onset of post-operative infections, prevent the appearance of cystoid macular oedema and improve ocular lubrication.
The use of eye drops in single-dose formulation is preferable, as the presence of preservatives and especially the presence of Benzalkonium chloride tends to increase the damage to the conjunctival mucosa.
In the early post-operative stages, it is good practice to use a cortisone-antibiotic combination, choosing a cortisone with high penetrability in the anterior chamber, to use NSAIDs to prevent cystoid macular oedema and artificial tears to improve the dyslacrimia that is very often present in the post-operative period. In some circumstances, in the presence of foreign body sensation symptoms, eye drops can also be used that have greater persistence in the eye and help to improve dyslacrimia.
Several studies compare the efficacy of cortisone-antibiotic combinations for topical use, demonstrating the equal efficacy of dexamethasone/netilmycin and dexamethasone/tobramycin. In favour of the former, however, the presence of single-dose formulations on the market and a lower rate of antibiotic resistance phenomena should be emphasised. In our opinion, this makes the dexamethasone/netilmycin combination the safest and most manageable for the treatment of cataract surgery patients (tables 1-4).
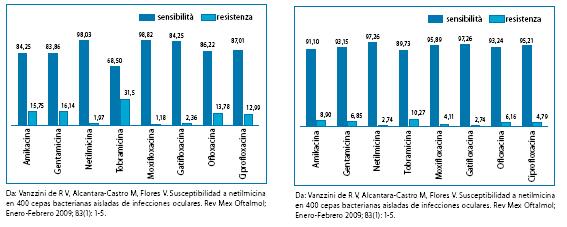
en 400 cepas bacterianas aisladas de infecciones oculares. Rev Mex Oftalmol;
Enero-Febrero 2009; 83(1): 1-5.
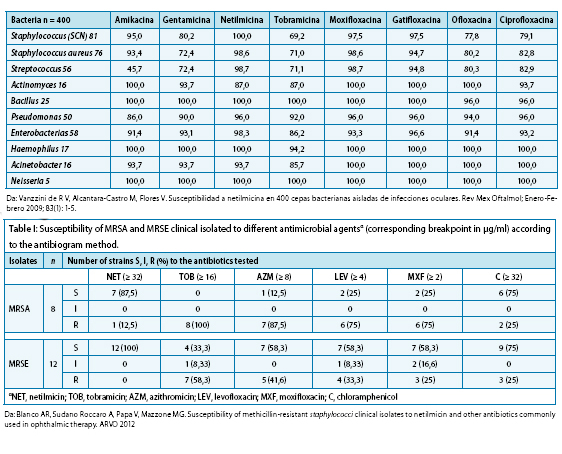
2009; 83(1): 1-5.
Conclusions
Cataract surgery is a traumatic event for the eye, which responds by generating inflammation. Both the inflammatory process following surgery and the severing of superficial nerve endings contribute to generating or worsening a dyslacrimia leading to ocular discomfort. Patients who had no tear film changes pre-operatively are those who suffer most from the onset of this problem post-operatively.
To avoid, or at least to minimise, the discomfort resulting from the onset of dry-eye, in addition to performing a flawless surgical procedure, it is advisable to carefully prepare the eye for surgery by treating inflammation and infection pre-operatively, to be precise in the surgical phase (do not overdo it with disinfectants, mydriatics, anaesthetics) and to manage the post-operative period with eye drops in single-dose formulation, always supplementing with an artificial tear.
Vincenzo Orfeo, Domenico Boccuzzi, Stefano Tarallo
Ophthalmology Operating Unit
Mediterranean Clinic - Naples
Bibliography
1. Cho YK, Kim MS. Dry eye after cataract surgery and associated intraoperative risk factors. Korean J Ophthalmol. 2009 Jun;23(2):65-73. doi: 10.3341/kjo.2009.23.2.65. Epub 2009 Jun 9.
2. Li XM, Hu L, Hu J, Wang W. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007 Oct;26(9 Suppl 1):S16-20.
3. Sun XG, Shi YY, Zhang C. [Not to ignore the dry eye of cataract patients after surgery]. Zhonghua Yan Ke Za Zhi. 2008 Apr;44(4):291-2.
4. Speaker MG, Milch FA, Shah MK, et al. Role of external bacterial flora in the pathogenesis of acute postoperative endophthalmitis. Ophthalmology 1991;98:639-49; discussion 650.
5. Ciulla TA, Starr MB, Masket S. Bacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based update. Ophthalmology 2002;109:13-24.
6. Speaker MG, Menikoff JA. Prophylaxis of endophthalmitis with topical povidone-iodine. Ophthalmology 1991;98:1769-75.
7. Carrim ZI, Mackie G, Gallacher G, Wykes WN. The efficacy of 5% povidone-iodine for 3 minutes prior to cataract surgery. Eur J Ophthalmol 2009;19:560-4.
8. Ferguson AW, Scott JA, McGavigan J, et al. Comparison of 5% povidone-iodine solution against 1% povidone-iodine solution in preoperative cataract surgery antisepsis: a prospective randomised double blind study. Br J Ophthalmol 2003;87:163-7.
Dr. Carmelo Chines
Direttore responsabile
