Carotid-cavernous fistulas (FCC) are abnormal communications between the carotids or branches thereof and the cavernous sinus (1,2). Although they represent a pathology of strict neuroradiological and neurosurgical relevance, the ophthalmologist is often called upon first because of the appearance of ocular signs and symptoms that, in non-eclectic cases, may be so blurred and non-specific as to completely mislead the correct diagnostic picture.
FCCs constitute approximately 10-15% of all intracranial arteriovenous malformations. They can be classified on the basis of three criteria:
–Pathogenetic (spontaneous and traumatic fistulas)
–Haemodynamic (high-flow and low-flow fistulas)
–Angiographic (direct and indirect or dural fistulas)
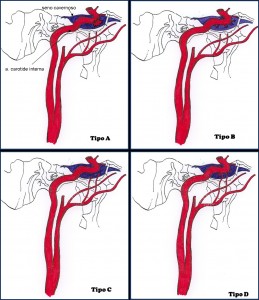
Barrow in 1985 distinguished them into type A fistulas (direct high-flow, high-pressure shunts that occur by rupture of the intracavernous tract of the internal carotid artery within the cavernous sinus) and type B, C and D fistulas, or dural fistulas (indirect low-flow, low-pressure shunts between the small meningeal branches of the internal carotid artery, the external carotid artery or both and the cavernous sinus) (fig. 1) (2).
While direct fistulas are mostly of a traumatic or iatrogenic nature, indirect fistulas are in most cases of spontaneous onset (1). Systemic vasculopathies (hypertension, diabetes, arteriosclerosis) and connective tissue disorders (elastic pseudoxanthoma, Marfan and Ehlers-Danlos syndrome) are predisposing factors.
In order to fully understand the aetiology of CCFs, as well as for a correct therapeutic approach, it is important to know the anatomy of the cavernous sinus with its afferents and efferences as well as the intracranial course of the carotids, with particular reference to the intracavernous course of the internal carotid artery.
Clinical manifestations
The mode of onset of FCC depends fundamentally on the drainage route taken. In the case of a direct fistula (Barrow's type A), the predominantly anterior drainage affects the upstream venous vessels (ophthalmic veins) with the striking appearance of a series of rather characteristic signs and symptoms involving the ocular apparatus (red-eyed syndrome)which therefore do not pose any major problems for diagnosis (3). If the drainage is predominantly posterior (supra- and inf. petrous sinuses), due, for example, to a concomitant thrombosis of the ophthalmic veins, the ocular congestive symptom picture will be more nuanced (white-eyed syndrome). The presence of communication with the contralateral cavernous sinus easily explains the appearance of ocular symptoms also, and in rare cases only, in the contralateral ocular apparatus.
The ocular signs that should lead one to suspect a FCC, when present simultaneously, are the conjunctival chemosiswhich may be barely noticeable or so marked that it prolapses through the palpebral fissure; thearterialisation of conjunctival and episcleral vesselswhich dilate, taking on a characteristically tortuous appearance, defined a "caput medusae'; the proptosis, ipsilateral to the fistula and pulsating in the case of a direct fistula, due to transmission of the sphygmic wave from the internal carotid artery to the dilated ophthalmic veins (fig. 2a, b); a breath, often reported by the patient himself, which can be heard by placing a phonendoscope over the affected eye. L'ocular hypertension is a sign that is almost always present and is induced by several factors, such as increased pressure in the episcleral veins, a reduction in the artero-venous pressure gradient resulting in hypoxia of the retinal tissues and the appearance of a neovascular type of glaucoma, engorgement of the choroidal vascular bed and oedema of the ciliary body, which can lead to an anterior thrust of the iris-lens diaphragm and the establishment of a pupillary block (4).
[caption id="attachment_1653" align="alignleft" width="300"] Ph. 2 a) patient with pulsating left proptosis; b) same patient, chemosis and conjunctival caput medusae; c and d) same patient after embolising treatment.[/caption]
Ph. 2 a) patient with pulsating left proptosis; b) same patient, chemosis and conjunctival caput medusae; c and d) same patient after embolising treatment.[/caption]
On examination of the ocular fundus, a dilation of retinal veins. Other less frequent findings are occlusion of the central retinal vein, oedema of the optic papilla and intraretinal haemorrhages.
The repercussion of this congestive situation on the functionality of the visual apparatus leads to the appearance of diplopia up to complete ophthalmoplegia, from direct compression of the nerve trunks within the sinus or from ischaemia secondary to flow alterations in the vasa nervorum (the abducens is the most affected nerve due to its location in the cavernous sinus which makes it more susceptible to compression). Orbital venous stasis can also contribute to the appearance of diplopia, inducing a thickening of the ocular muscles with consequent mechanical limitation of their motility. The visual impairment, later, occurs due to anterior ischaemic opticopathy, chronic retinal hypoxia, ocular hypertension or corneal changes.
Diagnosis
A direct FCC should be suspected in all those patients presenting with the sudden onset of proptosis associated with conjunctival chemosis and arterialisation of the episcleral vessels. When these manifestations appear after a head injury, the diagnosis should be obvious; even in the absence of a traumatic event, the rupture of an intracavernous aneurysm should always be considered. Similarly, the appearance of a similar, but more nuanced, symptomatology developing spontaneously in an adult subject, especially one suffering from systemic vasculopathies or connective tissue diseases, should lead one to look for the presence of a dural fistula. Since ocular signs in these cases are often misleading, as they can be confused with conjunctivitis, episcleritis, dysthyroidal orbitopathy, an inflammatory or neoplastic orbital process, imaging becomes essential (5,6).
Ocular ultrasonography, colour Doppler echo, magnetic resonance imaging (MRI) and angio-RM, highlighting indirect signs of the FCC, secondary to venous stasis and the reversal and arterialisation of flow in the orbital venous structures, serve to confirm the diagnostic hypothesis and justify the search for definitive confirmation by means of invasive investigations, such as selective angiography of the cerebral circulation. This examination, in addition to representing the only means at our disposal to highlight the site of the fistula and all the branches involved in its genesis, is indispensable if we decide to proceed with embolising treatment.
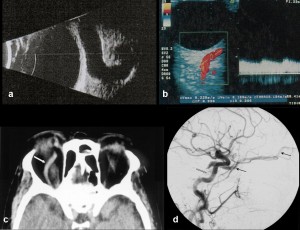
Ultrasound: In A-scan, dilated ophthalmic veins appear as lesions with a regular internal structure and low reflectivity. The lesion is demarcated by clear opening and closing echoes, corresponding to the walls of the dilated vessels. The A-scan investigation can also serve to demonstrate and quantify the thickening of the extrinsic ocular muscles. With B-scan ultrasonography, dilated ophthalmic veins appear as echopriate areas with clear margins in the context of a strongly reflecting retrobulbar tissue (1). In some sections, the dilated superior ophthalmic vein can sometimes be revealed in the form of a sinuous echopriva area (Fig. 3a).
Eco-colour dopplerIt is a non-invasive, reliable, sensitive method that can provide details of the haemodynamic characteristics of fistulas, showing dilatation of the superior ophthalmic vein, with arterialisation and reversal of flow within it (fig. 3b). This examination is of particular importance in low-flow dural fistulas, highlighting even very slight haemodynamic changes that would otherwise be undetectable with other methods. This technique also proves to be indispensable in the follow-up after embolization treatment, to demonstrate its efficacy, the stability of the result over time or the occurrence of any recurrence (1,7).
[caption id="attachment_1660" align="alignleft" width="300"] Ph 3 a) B-scan ultrasonography; b) echo-colordoppler; c) CT orbit; d) cerebral angiography (arterial phase): dural FCC starting from the meningeal branches of the ascending pharyngeal art (white arrow). Dilatation of the superior ophthalmic vein (black arrows).[/caption].
Ph 3 a) B-scan ultrasonography; b) echo-colordoppler; c) CT orbit; d) cerebral angiography (arterial phase): dural FCC starting from the meningeal branches of the ascending pharyngeal art (white arrow). Dilatation of the superior ophthalmic vein (black arrows).[/caption].
CT scan with mdcAt the endocranial level, a dilated venous sinus, which appears as a hyperdense parasellar mass with sharp and well-defined contours, with clear enhancement after M.D.C. (1). At the orbital level, dilatation of the superior and inferior ophthalmic veins and an increase in thickness and density of the ocular muscles can be appreciated (Fig. 3c).
RMshows dilatation of the cavernous sinus and ophthalmic veins, which appear signal-free in both T1-weighted and T2-weighted sequences. In cases with thrombosis in the cavernous sinus or ophthalmic veins, these structures will appear hyperintense in all sequences. In cases with posterior or superior drainage, the examination shows parenchymal cerebral oedema or a serpiginous pattern in the cortical veins.
Angio-RM: although it does not provide the same spatial resolution as selective angiography, due to the relative difficulty in highlighting small fistulas, it can nevertheless be used to highlight larger vascular anomalies or monitor the behaviour of those already diagnosed.
Cerebral angiographyselective digital angiography of the cerebral circulation represents an invasive investigation, involving selective bilateral catheterisation of both carotids. It constitutes the only instrumental investigation capable of directly visualising the fistula (fig. 3d); moreover, thanks to the demonstration of all the afferents involved and the drainage pathways, it appears irreplaceable for making a prognostic judgement and for setting embolising treatment.
Treatment
The aim of FCC therapy is to resolve the clinical picture with minimal risk to the patient (Fig. 2c, d). From a conceptual point of view, the 'cure' in fistulas is the complete closure of the abnormal communication between arteries and veins; as these are often multiple communications, however, this goal is often difficult to achieve. However, the important end result is the clinical one, given by the resolution or improvement of symptoms, and not the angiographic one; in fact, a subtotal occlusion is often sufficient to resolve the clinical picture.
Treatment options for fistulas vary from simple monitoring, to compression manoeuvres on the carotids or jugulars, to embolisation therapy by trans-arterial or trans-venous route, to radiotherapy (8). Less widely used are electrothrombosis and direct surgical treatment.
The simple monitoring is advisable in dural fistulas that do not present disabling symptoms or signs of threatened visual impairment or signs of posterior drainage with risk of even fatal cerebral haemorrhage. In fact, in a variable percentage of 10% to 60%, these fistulas may spontaneously resolve, sometimes after an angiography has been performed for diagnostic purposes (possibly due to a vascular spasm favouring thrombosis).
In patients with symptomatic dural fistulas, without signs of impaired visual function or cortical drainage, the manual carotid-jugular compression (9). This technique consists of compressing the carotid-jugular trunk for 10 sec every hour in order to slow the flow through the fistula and promote thrombosis. This manoeuvre may also be helpful in those cases where complete closure of the fistula has not been achieved with embolisation. The compression manoeuvre is not without risk, however, especially in patients who have significant carotid atherosclerosis or who have had ischaemic or syncopal episodes in the past.
The embolising treatment is the elective therapy in direct fistulas and dural fistulas, in which there has been no spontaneous resolution or with compression manoeuvres. Embolisation can be performed via the trans-arterial (femoral artery) or trans-venous (femoral vein) route and consists of introducing substances capable of inducing a thrombotic event at the fistula site.
For ease of access and excellent results, the approach through the inferior petrous sinus is the treatment of choice. In cases where this is not accessible because it cannot be seen radiologically or in cases where it is particularly tortuous or does not have a direct connection with the internal jugular, the superior ophthalmic vein is used (10).
The radiotherapy has proved to be a useful therapeutic tool in dural fistulas unsuccessfully treated with common endovascular methods. Its therapeutic efficacy is probably linked to the development of an inflammatory process in the wall of the irradiated vessels resulting in thrombosis.
L'electrothrombosis consists of introducing a copper or bronze wire into the cavernous sinus to which an electric current is applied until thrombosis is induced.
Conclusions
FCCs represent a pathology of ophthalmological interest characterised by ocular signs that are not always pathognomonic, but are sometimes subtle and difficult to interpret, so much so that they often create problems of differential diagnosis. Failure or delayed treatment can lead, in some cases, to serious and sometimes irreparable complications.
Prof. Ennio Polito
Director of the School of Specialisation
at the University of Siena
Bibliography
1) de Keizer R. Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit. 2003 Jun;22(2):121-42
2) Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT.Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985 Feb;62(2):248-56
3) Phelps CD, Thompson HS, Ossoinig KC. The diagnosis and prognosis of atypical carotid-cavernous fistula (red-eyed shunt syndrome). Am J Ophthalmol. 1982 Apr;93(4):423-36
4) Jørgensen JS, Guthoff R. The role of episcleral venous pressure in the development of secondary glaucomas Klin Monatsbl Augenheilkd. 1988 Nov;193(5):471-5
5) Loré F, Polito E, Cerase A, Bracco S, Loffredo A, Pichierri P, Talidis F. Carotid cavernous fistula in a patient with Graves' ophthalmopathy. J Clin Endocrinol Metab. 2003 Aug;88(8):3487-90.
6) Oestreicher JH, Frueh BR. Carotid-cavernous fistula mimicking Graves' eye disease. Ophthal Plast Reconstr Surg. 1995 Dec;11(4):238-44
7) Duan Y, Liu X, Zhou X, Cao T, Ruan L, Zhao Y. Diagnosis and follow-up study of carotid cavernous fistulas with color Doppler ultrasonography: analysis of 33 cases. J Ultrasound Med. 2005 Jun;24(6):739-45
8) Théaudin M, Saint-Maurice JP, Chapot R, Vahedi K, Mazighi M, Vignal C, Saliou G, Stapf C, Bousser MG, Houdart E. Diagnosis and treatment of dural carotid-cavernous fistulas: a consecutive series of 27 patients. J Neurol Neurosurg Psychiatry. 2007 Feb;78(2):174-9
9) Higashida RT, Hieshima GB, Halbach VV, Bentson JR, Goto K. Closure of carotid cavernous sinus fistulae by external compression of the carotid artery and jugular vein. Acta Radiol Suppl. 1986;369:580-3
10) Klink T, Hofmann E, Lieb W. Transvenous embolization of carotid cavernous fistulas via the superior ophthalmic vein. Graefes Arch Clin Exp Ophthalmol. 2001 Aug;239(8):583-8
11) Meyers PM, Halbach VV, Dowd CF, Lempert TE, Malek AM, Phatouros CC, Lefler JE, Higashida RT. Dural carotid cavernous fistula: definitive endovascular management and long-term follow-up. Am J Ophthalmol. 2002 Jul;134(1):85-92