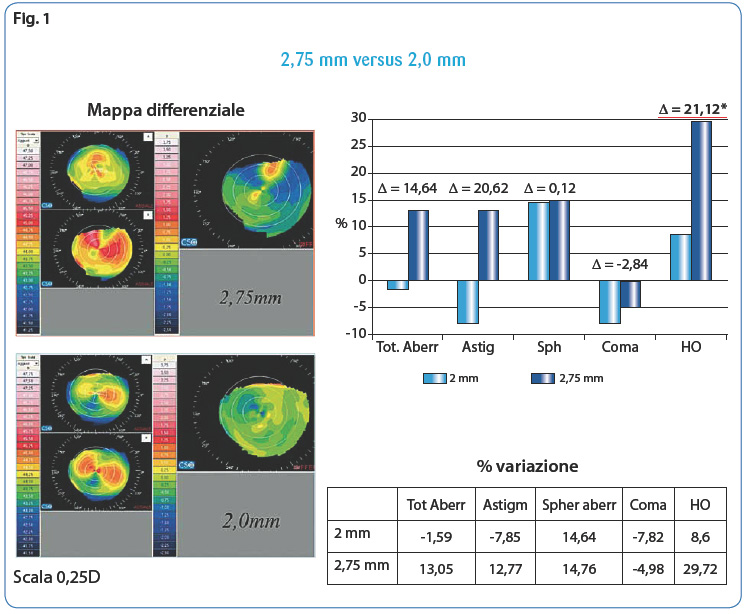
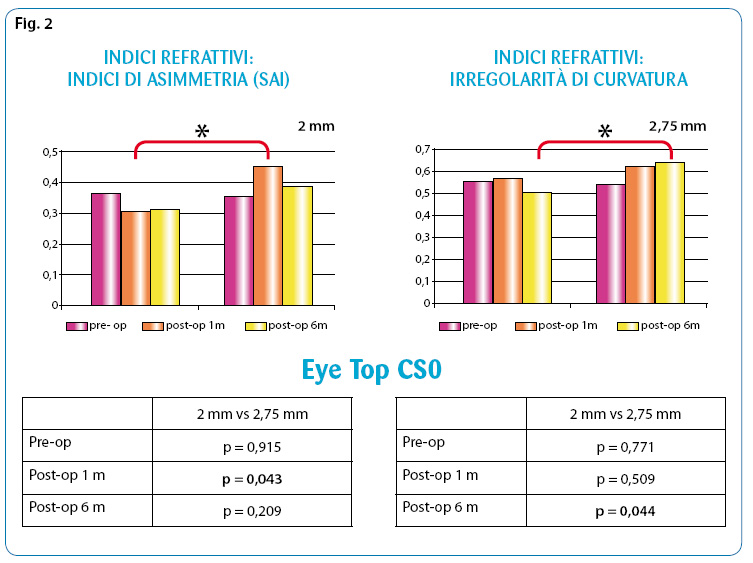
With regard to refractive indices, we have also shown that the asymmetry index (SAI) is lower with the 2 mm incision, while the surface irregularity is higher with the 2.75 mm incision (Fig. 2).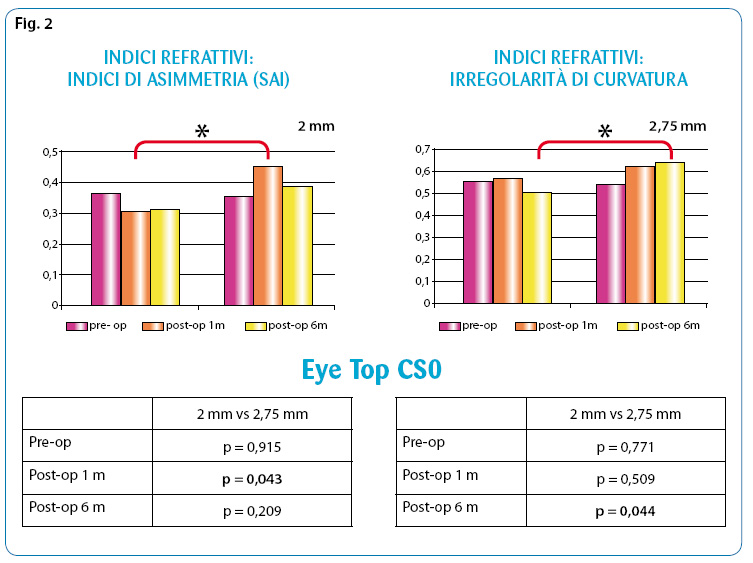
IOL and vision quality Regarding the relationship between intraocular lens and quality of vision it can be stated that the IOLs, in relation to the geometry of the optics, which varied in shape (equibiconvex, flat-convex anterior or posterior), radius of curvature and edge characteristics (square edge or round edge), manifested variable visual results with respect to the aberrometric phenomenon and the glare(4). In fact, the quantitative measurement of visual acuity with the optotype alone cannot fully express visual functionality, but must be combined with the measurement of contrast sensitivity and ocular aberrations.(5). The presence of any defect in the optical system, from the tear film to the retina, which produces a distortion of light rays or an imperfect focusing of images on the retina, generates vision alterations(6). And all this also applies in the pseudophakic patient. With regard to the contrast sensitivityit has been shown to decrease physiologically with age: this phenomenon is due to the increase in total aberrations in the eye(7). Furthermore, when contrast sensitivity is reduced after cataract surgery, the quality of vision is also reduced and consequently so is the ability to read or see at night(8). There is also evidence that the performance of newly designed IOLs is better under both photopic and mesopic conditions(9,10). In addition to improving contrast sensitivity, the study of newly designed IOLs aims to reduce optical aberrations, which are also responsible for suboptimal vision.
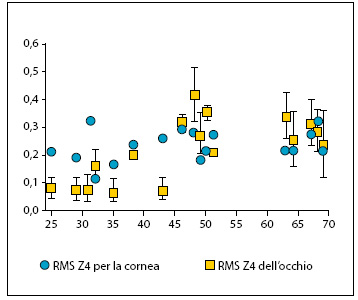
Intraocular aberrations and clinical practice In clinical practice, the magnitude of ocular aberrations is measured with an aberrometer, expressed in microns and represented in an aberrometric map(11). So far, the use of the aberrometer has mainly been in the field of corneal refractive surgery, as a diagnostic tool to allow specific customised surgery. Currently, the study of aberrations also extends to the pre- and postoperative management of cataract surgery, to assess any aberrations induced by the various types of implanted IOLs. In the study of pseudophakic patients, the most important aberration is thespherical aberration (Z4,0). This is a symmetrical aberration whereby light rays passing through the paraxial (central) pupil zone focus at a different distance than those passing through the marginal (lateral) pupil. By convention, spherical aberration is positive when the marginal rays come into focus before the paraxial ones, while it is negative when the opposite occurs. The difference between the marginal and paraxial focal point is called longitudinal spherical aberration(12). The study of optical aberrations led to the construction of New generation aspherical IOLs. The crystalline of a young subject has a negative spherical aberration because its refractive index is lower in the periphery than near the visual axis. From the age of 40, the crystalline lens shows significant aberrometric changes from negative to positive over the years(13). On the other hand, the cornea is a normally prolate surface, i.e. it has a lower refractive power in the periphery than in the central zone, which is responsible for the formation of positive spherical aberrations. In contrast to the crystalline lens, the cornea is an optical system that remains relatively stable over the years so its positive spherical aberration does not change. Thus, the crystalline lens physiologically not only loses its ability to compensate for corneal aberrations, but also increases the positive corneal aberrations of the ocular system, thus leading to a deterioration of optical quality with age.(14) (Fig. 3).
[caption id="attachment_1694" align="aligncenter" width="358"]
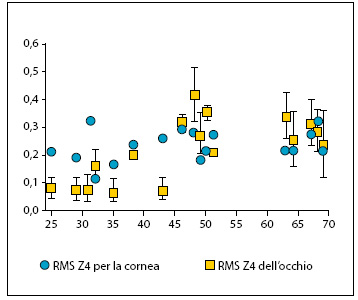
Fig. 3. Corneal aberrations (+) remain constant over time[/caption].
IOLs with spherical morphology, i.e. with both surfaces of the optic body spherical, introduce a positive spherical aberration which, when added to the corneal aberration, can contribute to reduced visual quality after cataract surgery(15). Technological advances in cataract surgery and the development of IOL new design led to the development of aspherical lenses developed for compensate and cancel the positive spherical aberration of the cornea. Currently, there are several IOL models on the market with a different measure of asphericity correction. Many studies have demonstrated the effectiveness of aspheric IOL designs in correcting positive spherical corneal aberrations (15,16) and improve contrast sensitivity accordingly(10,17,18,19). Aspherical IOLs improve contrast sensitivity in both mesopic and photopic conditions (10,20,21). Many studies have compared the contrast sensitivity obtained with the implantation of aspherical IOLs and spherical IOLs (12,19,20) showing an improvement with aspherics(17). Only two studies showed no difference between aspheric and spherical IOLs in terms of low and high-contrast visual acuity and contrast sensitivity(24,25). These differences in results between the various studies could be explained by the different tests, charts or instruments used to measure contrast sensitivity.(26). The current market already foresees aspheric IOLs at 41.8% and in the coming years at 54.9%(27).
Aspherical IOLs and OCPs OCP still represents one of the major postoperative complications following phacoemulsification surgery with IOL implantation in the sac, although the incidence, which may depend on numerous factors including surgical technique, IOL design and IOL optics material, is declining dramatically (28,29). Its development is a consequence of the proliferation and migration of Lenticular Epithelial Cells (Lecs) in the space between the posterior surface of the IOL and the posterior capsule. Normally, capsulorhexis allows for the sequestration and proper stabilisation of the IOL within the sac, reducing the incidence of capsular opacification. In this way, the IOL comes into contact with the inner surface of the residual anterior capsule, and especially with the lenticular epithelial cells. The reported consequences are reduced visual acuity and halo and glare phenomena. Much progress has been made in reducing postoperative OCP through modification of the IOL design. In fact, Nishi et al. demonstrated that an optical body with a square edge causes reduced OCP compared to an optical body with a rounded edge(30)This is because the 'edge effect' is intended to place a physical barrier to cell migration. Regarding, on the other hand, the asphericity of the IOL, in a 2011 study, it was shown that the incidence of OCP does not change significantly between spherical and aspherical IOLs(31). Conversely, the lens material influences the onset of posterior capsule opacification(32). In particular, the use of acrylic lenses seems to be associated with a lower incidence of OCP, so much so that most surgeons (ASCRS = 69% and ESCRS = 75%) prefer acrylic as the best lens material(27).
Prof. Aldo Caporossi
Director Complex Ophthalmology Unit
Department of Odontostomatological and Ophthalmological Sciences, University of Siena
Dr Gianluca Martone, Dr Patrizia Pichierri, Dr Patrizia Sergio
Department of Odontostomatological and Ophthalmological Sciences, University of Siena
Bibliography
1. Frezzotti R, Caporossi A, Mastrangelo D, Hadjistilianou T, Tosi P, Cintorino M, Minacci C. Pathogenesis of posterior capsular opacification. Part II: Histopathological and in vitro culture findings. J Cataract Refract Surg. 1990;16:353-60.
2. Samuelson SW, Koch DD, Kuglen CC. Determination of maximal incision length for true small-incision surgery. Ophthalmic Surg. 1991;22:204-7. 3. Uchio E, Ohno S, Kusakawa T. Spherical aberration and glare disability with intraocular lenses of different optical design. J Cataract Refract Surg 1995;21:690-696.
4. Applegate RA, Marsack JD, Ramos R, Sarver EJ. Interaction between aberrations to improve or reduce visual performance. J Cataract Refract Surg. 2003;29:1487-95.
5. Artal P, Ferro M, Miranda I, et al. Effects of aging in retinal image quality. J Opt Soc Am 1993;10:1656-62.
6. Ginsburg AP. Contrast sensitivity and function. Int Ophthalmol Clin 2003;43:5-16.
7. Aggarwal A, Khurana AK, Nada M. Contrast sensitivity function in pseudophakics and aphakics. Acta Ophthalmol Scand 1999;77:441-3.
8. Ricci F, Scuderi G, Missiroli F, et al. Low contrast visual acuity in pseudophakic patients implanted with an anterior surface modified prolate intraocular lens. Acta Ophthalmol Scan 2004;82:718-22.
9. Mierdel P, Kaemmer M, Mroche M et al. Ocular optical aberrometer for clinical use. J Biomed Opt 2001;6:200-4.
10. Charman WN, Chateau N. The prospects for super-acuity: limits to visual performance after correction of monochromatic ocular aberration. Ophthalmic Physiol Opt. 2003;23:479-93.
11. Wang L, Koch DD. Effect of decentration of wavefront-corrected intraocular lenses on the higher-order aberrations of the eye. Arch Ophthalmol 2005;123:1226-30.
12. Artal P, Berrio E, Guirao A, Piers P. Contribution of the cornea and internal surfaces to the change of ocular aberrations with age. J Opt Soc Am A Opt Image Sci Vis 2002;19:137-43.
13. Mester U, Dillinger P, Anterist N. Impact of a modified optic design on visual function: clinical comparative study. J Cataract Refract Surg 2003;29:652-60.
14. Chantra S, Pachimkul P, Naripthaphan P. Wavefront and ocular spherical aberration after implantation of different types of aspheric intraocular lenses based on corneal spherical aberration. J Med Assoc Thai. 2011;94 Suppl 2:S71-5.
15. Bellucci R, Scialdone A, Buratto L, et al. Visual acuity and contrast sensitivity comparison between Tecnis and AcrySof SA60AT intraocular lenses; a multicenter randomised study. J Cataract Refract Surg 2005;31:712-7.
16. Packer M, Fine IH, Hoffman RS. Wavefront technology in cataract surgery. Curr Opin Ophthalmol. 2004;15:56-60.
17. Caporossi A, Martone G, Casprini F, Rapisarda L. Prospective randomized study of clinical performance of 3 aspheric and 2 spherical intraocular lenses in 250 eyes. J Refract Surg 2007;23:639-48.
18. Casprini F, Balestrazzi A, Tosi GM, et al. Optical aberrations in pseudophakic eyes after 2.5-mm Nd:YAG laser capsulotomy for posterior capsule opacification. J Refract Surg 2008;24:702-6.
19. Morales EL, Rocha KM, Chalita MR, Nosé W, Avila MP. Comparison of optical aberrations and contrast sensitivity between aspheric and spherical intraocular lenses. J Refract Surg. 2011;27:723-8.
20. Packer M, Fine IH, Hoffman RS, Piers PA. Improved functional vision with a modified prolate intraocular lens. J Cataract Refract Surg 2004;30:986-992.
21. van Gaalen KW, Koopmans SA, Jansonius NM, Kooijman AC. Clinical comparison of the optical performance of aspheric and spherical intraocular lenses. J Cataract Refract Surg. 2010;36:34-43.
22. Kurz S, Krummenauer F, Thieme H, Dick HB. Contrast sensitivity after implantation of a spherical versus an aspherical intraocular lens in biaxial microincision cataract surgery. J Cataract Refract Surg 2007;33:393-400.
23. Munoz G, Albarran-Diego C, Montes-Mico R, et al. Spherical aberration and contrast sensitivity after cataract surgery with the Tecnis Z9000 intraocular lens. J Cataract Refract Surg 2006;32:1320-7.
24. Packer M, Ginsburg AP. Testing and reporting contrast sensitivity. J Cataract Refract Surg 2007;33:359-60.
25. Schaumberg DA, Dana MR, Christen WG, Glynn RJ. A systematic overview of the incidence of posterior capsule opacification. Ophthalmology 1998;105:1213–21.
26. Apple DJ, Solomon KD, Tetz MR, et al. Posterior capsule opacification. Surv Ophthalmol 1992;37:73-116.
27. Nishi O, Nishi K, Wickstrom K. Preventing lens epithelial cell migration using intraocular lenses with sharp rectangular edges. J Cataract Refract Surg 2000;26:1543-9.
28. Nanavaty MA, Spalton DJ, Gala KB, Dhital A, Boyce J. Effect of intraocular lens asphericity on posterior capsule opacification between two intraocular lenses with same acrylic material: a fellow-eye study. Acta Ophthalmol. 2011 Nov 8.
Dr. Carmelo Chines
Direttore responsabile