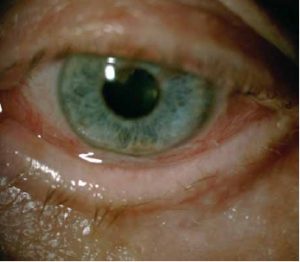
Under physiological conditions, the eyeball is protected and covered by a community of non-pathogenic microorganisms, the ocular microbiome. However, in the event of penetrating, accidental, surgical or injection-associated trauma, the injury that is generated can facilitate the migration of these micro-organisms within the eye itself, with the following infectious outcome. Suffice it to say that up to 82% of the post-cataract endophthalmitis are caused by the same microbial communities that populate the eye, an estimate that underlines the need for know and monitor the distribution of these ocular micro-organisms and their possible antibiotic resistance.
Le eye infections can be of varying nature, complexity and severity. The conjunctivitis bacterial is probably the most common infection, while the most serious, but less common, is theendophthalmitiswhich, in most cases, is due to a complication of eye surgery, trauma or intravitreal injections. However, although endophthalmitis is considered a rare complication, with an estimated occurrence of around 0.03-0.2% after cataract surgery and of 0.02-0.2% after a single intravitreal injectionThe high volume of such operations performed worldwide means that there are thousands of cases of endophthalmitis every year.
In order to limit the serious clinical effects that ocular infections can induce, especially in the post-operative setting, ophthalmic surgeons use topical antibiotics. data on their use over the years have not changed at all, in fact, in both a 2001 and a 2014 survey, it was found that about 90% of surgeons use this type of prophylaxis in both peri-operative and pre-operative settings.
But what are the most important rules to limit the occurrence of eye infections, especially those due to multi-resistant bacteria?
Certainly, it turns out the choice of antibiotic is crucialwhich depends on a multitude of factors; important considerations are clearly the spectrum of action and the evaluation of regional resistance patterns. Furthermore, a key aspect of antimicrobial prescribing is to ensure the use of antimicrobials in the correct dosage and for the optimal' duration of the treatment. In fact, using too low a dose, the so-called sub-therapeutic dose, the development of drug resistance may be accelerated. Similarly, resistance may be promoted by too short a duration of antimicrobial treatment.
In ophthalmic fieldFurthermore, in the light of the new protocols of the pharmacokinetic and pharmacodynamic parameters (PK/PD), not systemic but local, it would be important to re-evaluate the most commonly used antibiotics in clinical practice to ensure that they are used as efficiently as possible
Another important criterion for avoiding eye infections due to resistant bacteria is to be able to identify in advance patients who, due to their inherent characteristics, have a high risk of severe post-operative endophthalmitis. In particular, several studies have attempted to stratify and quantify the distribution of microbial resistancebacteria that are not sensitive to the major antibiotic classes used in clinical practice, in specific populations. The results showed an increased susceptibility of the following subjects:
- i health professionals, in which a high prevalence of MRSA strains (methicillin-resistant Staphylococcus aureus)
- i elderly subjectsover 80 years of age, a higher prevalence of MRSA, but also of methicillin-resistant Coagulase-negative Staphylococci (CoNS) was also found in this sub-population
- i individuals with diabetes mellitus.
In addition, they were identified as risk factors predisposing to increased colonisation with antibiotic-resistant strains, thealcohol abuse, the Behcet's disease and pre-operative antibiotic prophylaxis in the case of treatments administered with intravitreal injections, although the latter is still a debated factor.
The microbial resistance is a topical and highly relevant issue, and there is certainly a need for in-depth study and research into prevention, identification and treatment of resistant and multi-resistant bacteria. Unfortunately, today, most of this research is focused on systemic infections, and it may be some time before innovation in diagnostic and prevention methods can fully involve the ophthalmological field as well.
However, being able to distinctionto know correctly which antibiotics should be used and in which situations, and prescribe in accordance with the international microbiological guidelines, already allows the specialist to curb the problem, achieving high concentrations in the target tissue and maintaining sufficient duration of effects to reduce resistance phenomena.
Bibliography
- Grzybowski A et al. Microbial flora and resistance in ophthalmology: a review. Graefes Arch Clin Exp Ophthalmol. 2017 Feb 22. doi: 10.1007/s00417-017-3608-y. [Epub ahead of print].
- Schwartz SG, et al. Antibiotic prophylaxis: different practice patterns within and outside the United States. Clin Ophthalmol 2016; 10:251
- Dar OA et al. Exploring the evidence base for national and regional policy interventions to combat resistance. Lancet 2016. doi:10.1016/S0140- 6736(15)00520-6
Dr. Carmelo Chines
Direttore responsabile
