Le eye infections of bacterial aetiology, from the most common -blepharitis, conjunctivitis- to the more complex -keratitis, endophthalmitis- have a important impact on quality of vision and quality of life. For this reason, antibiotics are an essential tool in combating this type of infection. Unfortunately, today we are increasingly seeing an increase in the number of clinical failures or sub-optimal outcomes following the empirical treatment of eye infections with different classes of antibiotics. This is due to excessive and, many times, inappropriate use that has facilitated the development of resistance. Finally, it should be added that, to date, there is no national or international surveillance service for antimicrobial resistance of common and non-common ocular pathogens, which makes difficult determine the true prevalence of antibiotic resistance.
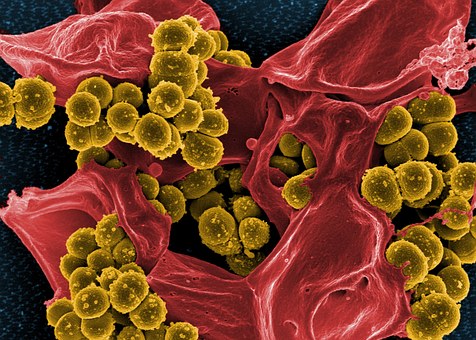 In this respect, the data discussed here come mainly from epidemiological and antibiotic resistance analyses of ocular pathogens carried out by various studies, the most important of which is certainly theARMOR (Antibiotic Resistance Monitoring in Ocular micRoorganisms). This study, active in the United States since 2009, showed a high level of antibiotic resistance in ocular infections and in particular among ocular isolates of Staphylococcus aureus and Coagulase Negative Staphylococci (CoNS). Among these isolates, the 87% of the S.aureus methicillin-resistant (MRSA) and 77% of methicillin-resistant CoNS (CoNSMR) showed resistanceas well as methicillin, to several antibiotics at the same time. These bacteria are called multi-drug resistant (MDR).
In this respect, the data discussed here come mainly from epidemiological and antibiotic resistance analyses of ocular pathogens carried out by various studies, the most important of which is certainly theARMOR (Antibiotic Resistance Monitoring in Ocular micRoorganisms). This study, active in the United States since 2009, showed a high level of antibiotic resistance in ocular infections and in particular among ocular isolates of Staphylococcus aureus and Coagulase Negative Staphylococci (CoNS). Among these isolates, the 87% of the S.aureus methicillin-resistant (MRSA) and 77% of methicillin-resistant CoNS (CoNSMR) showed resistanceas well as methicillin, to several antibiotics at the same time. These bacteria are called multi-drug resistant (MDR).
Other studies have confirmed a progressive increase in antibiotic resistance in eye infectionsin particular, of the blocks CoNS against specific classes of antibiotics, such as fluoroquinolones, to which MRSA and S.epidermidis methicillin-resistant (MRSE), show rates of resistance >75%. On the other hand, fortunately these studies have shown a high sensitivity (approximately 90%) for both MRSA and MRSE to molecules such as netilmycin, vancomycin and cefuroxime.
To these analyses is added a European surveillance study on the activity of aminoglycosides and fluoroquinolones against ophthalmic pathogens. The study showed that antibiotic resistance rates depend by microbial species e by area (country) in which these resistances arise. Resistance to ciprofloxacin, tobramycin, erythromycin and, to a lesser extent, chloramphenicol, is characteristic of all staphylococci. Multi-resistance has been frequently found in MRSA and MRCoNS; whereas S. pneumoniae, H. influenzae e P. aeruginosa were frequently resistant to erythromycin, beta-lactams and ciprofloxacin/tobramycin, respectively. Antimicrobial resistance rates showed substantial differences in the different European countries analysed in the study, further confirming the importance of considering local epidemiology for the empirical management of eye infections.
The antibiotic resistance data from the studies discussed here emphasise the need for specialists in the field to develop practical and prudent strategies in the administration of topical antimicrobial therapies that take into account national surveillance data in order to use targeted molecules for less empirical and more personalised therapy.
Finally, the stability of its efficacy over time should also be considered when choosing an antibiotic. In ophthalmology, among the various antibiotic molecules available, one distinguishes between netimycin limited use both systemically and topically, maintained its effectiveness showing unchanged susceptibility data for the last 20 years against the main ocular pathogens, including MRSA and MRSEwith values comparable only to molecules such as cefuroxime and vancomycin, both of which are not available for topical use.
Bibliography
-Asbell P.A. et al. Antibiotic resistance among ocular pathogens in the United States: five-year results from the Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) Surveillance study. JAMA Ophthalmol.
-ESCRS Guidelines for Prevention and Treatment of Endophthalmitis Following Cataract Surgery: Data, Dilemmas and Conclusions 2013.
-Jack D. Stringham et al. Trends in Fluoroquinolone Nonsusceptibility Among Coagulase-Negative Staphylococcus Isolates Causing Endophthalmitis, 1995-2016. JAMA Ophthalmol. 2017.
-Blanco AR et al. Susceptibility of methicillin-resistant Staphylococci clinical isolates to netilmycin and other antibiotics commonly used in ophthalmic therapy. Curr Eye Res. 2013.
-Papa V et al. Ocular flora and their antibiotic susceptibility in patients having cataract surgery in Italy. J Cataract Refract Surg. 2016.
-Sanfilippo C.M et al. Surveillance of the Activity of Aminoglycosides and Fluoroquinolones Against Ophthalmic Pathogens from Europe in 2010-2011. Current Eye Research 2015.
Dr. Carmelo Chines
Direttore responsabile
