This article reviews the surgical options for correcting presbyopia through the techniques available to achieve multifocality.
Introduction
Accommodation refers to the change in the dioptric power of the eye that enables us to focus both near and far(1). Presbyopia is the loss of the power of accommodation, which begins fairly early in life, but becomes clinically manifest around the age of 40.(1)making people dependent on wearing glasses for near vision.
Correcting presbyopia has always been a challenge for refractive surgeons because we are not yet able to achieve full restoration of accommodative power and have to fall back on pseudo-accomodative procedures, which improve near vision through the induction of multifocality or through increased depth of field (2).
It is estimated that, by 2020, 1.37 billion people will be presbyopic(3)Therefore, correction of this refractive condition is a necessity due to its negative impact on quality of life(4) and since it constitutes an economic burden(5).
Presbyopia can be surgically corrected at the level of the cornea with procedures such as LASIK monovision, micro-monovision, presbyLASIK, Laser Blended Vision and corneal inlays; with regard to the type of intraocular lenses, it can be corrected with multifocal IOLs or EDOF (Extended Depth Of Focus) IOLs, or with phakic multifocal IOLs. The choice of procedure will depend on the patient's age, expectations, daily activities and any comorbidities.
In this article, we will discuss surgical options for correcting presbyopia.
Corneal procedures
Current corneal procedures for the correction of presbyopia are: LASIK monovision, micro-monovision, presbyLASIK, Laser Blended Vision and corneal inlays. The main advantages of these procedures are their reversibility, minimally invasive nature, and the fact that they are the ideal solution for young presbyopes (<50 years). Ancillary tests such as corneal topography and ultrasound pachymetry are necessary prior to surgery; patients with thin corneas or corneal ectasia are not good candidates for these procedures.
Monovision LASIK and micro-monovision
Monovision is an induced anisometropia, in which the non-dominant eye is corrected for near vision and the dominant eye is corrected for distance vision. The degree of anisometropia increases in relation to the patient's age (from -1.25 diopters (D) in a 40-year-old patient to 2.50 D in a 65-year-old)(6). One of the main limitations of monovision is the loss of stereopsis, which correlates with the degree of anisometropia.
In micro-monovision, the induced anisometropia in the non-dominant eye ranges from-1.00 to -1.5 D while the refractive target is "plano" (absence of refractive error) in the dominant eye, irrespective of the patient's age(7). This degree of anisometropia allows the patient to retain sufficient stereopsis. (8).
Monovision is contraindicated in patients with strabismus, strong ocular dominance(9)truck or taxi drivers and airline pilots(6).
The simplicity, good clinical results, and potential reversibility with a retouch using the excimer laser make mono- and micro-monovision very effective and widely used by refractive surgeons.
PresbyLASIK
PresbyLASIK is an excimer laser procedure that creates a multifocal corneal surface(10)using two main techniques: central and peripheral presbyLASIK. In peripheral presbyLASIK, a central oblate zone is created for distance vision and a peripheral prolate zone for near vision(8). In the central presbyLASIK, a central hyperpositive area is created for near vision, while the periphery is intended for distance vision(10) (Fig. 1).
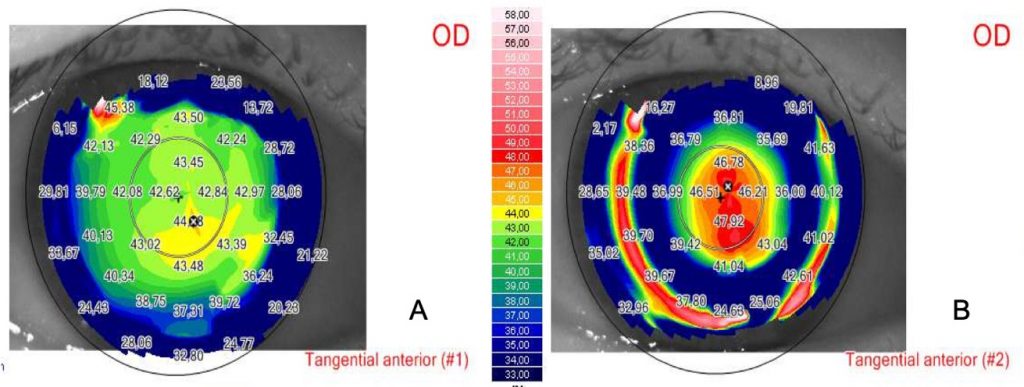
Since peripheral presbyLASIK involves ablation of a significant amount of corneal tissue in order to create a hyperprolate form, the most widely used technique is central presbyLASIK(11).
Available software for central presbyLASIK includes: PresbyMAX (SCHWIND eye-tech-solutions GmbH, Kleinostheim, Germany), SUPRACOR (Technolas Perfect Vision GmbH, Munich, Germany), and AMO Visx hyperopia-presbyopia multifocal approach (AMO Development LLC, Milpitas, California).
The PresbyMAX software was developed by J. Alió and S. Arba; it can be used in emmetropic, myopic and hypermetropic patients with good results for near and far (12-16).
Although both techniques improve near vision, there is a loss of lines in distance vision (17).
Laser Blended Vision
Laser Blended Vision combines a low degree of asphericity and micro-monovision in each eye to achieve good near and far distance. This technique provides good visual results both near and far and can be used in hypermetropes, myopes and emmetropes (18-20).
We define 'hybrid' as techniques based on the combination of monovision and corneal multifocality; LBV, Supracor and PresbyMAX software fall into this group of hybrid techniques and have improved corneal multifocality results.(21)
Intracorneal inlays
Intracorneal inlays have the advantage of being minimally invasive and reversible; moreover, they are easy to implant, although their use has been questioned because of the reduction in contrast sensitivity and distance visual acuity as well as the risk of corneal opacity. All intracorneal inlays must be centred on the first Purkinje reflex(22)and implanted under a stromal flap or within a stromal sac created with the femtosecond laser(23) in the non-dominant eye(24) (Fig. 2).
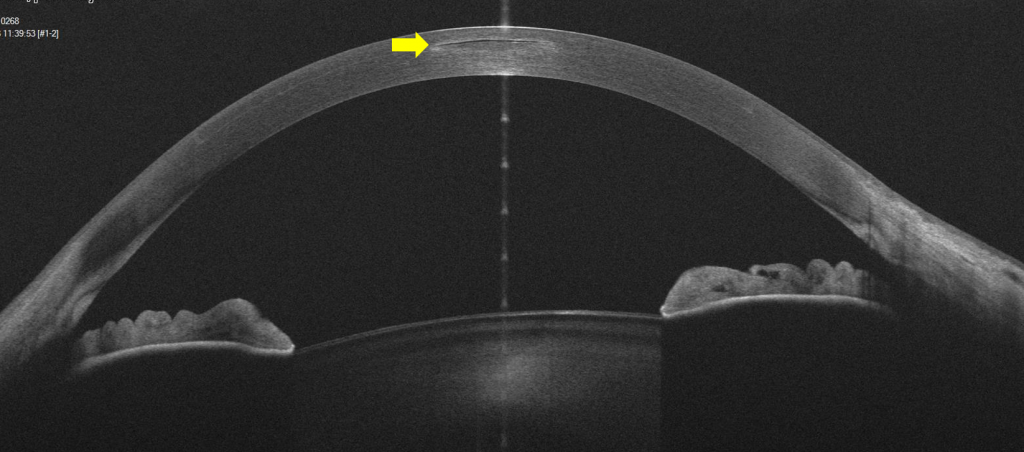
Three different types of intracorneal inlays have been developed: corneal remodelling inlays, refractive inlays and small aperture inlays. We will discuss the latter as they are the most widely implanted inlays.(22)Inlays for corneal remodelling (such as Raindrop, Revision Optics, Lake Forest, California, USA) are now off the market due to an increased risk of corneal opacity and loss of distance visual acuity; and refractive inlays (Flexivue, Presbia, Los Angeles, California, USA, Icolens, Neoptics AG, Hunenberg, Switzerland) have shown mixed results that have limited their clinical use.
Kamra
The Kamra inlay (Acufocus, Irvine, California, USA) improves near vision by increasing depth of focus; it is an opaque inlay with a diameter of 3.8 mm, a central aperture of 1.6 mm and 8,400 microperforations that
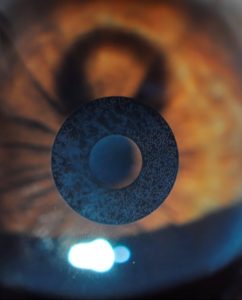
allow an adequate nutritional supply through the cornea(25) (Fig. 3).
It can be implanted simultaneously with the LASIK procedure in myopic, hypermetropic and emmetropic patients, resulting in improved near and intermediate distance visual acuity26,27). Some complications that can occur after Kamra inlay implantation are: opacity, photophobia, blurred vision, halos and refractive shifts(28-30)These complications have limited its use.
Multifocal Intraocular Lenses and EDOF (Extended Depth of Focus)
Replacing the crystalline lens with a premium IOL is the most decisive option for correcting presbyopia as this type of intraocular lens corrects distance, intermediate distance and near vision. They are the best option for hypermetropes over the age of 50, and for myopes over the age of 55.
Multifocal IOLs were introduced in the 1980s and since then, their design has been improved in order to induce less dysphotopsia while maintaining good visual acuity.
Assessments before multifocal IOL implantation
Careful patient selection is indispensable for good results.
Patients with type A personality as well as extremely demanding patients are not good candidates for implantation of a multifocal IOL. Patients with ophthalmological conditions that result in reduced contrast sensitivity, such as advanced glaucoma or macular pathologies, are not good candidates for implantation of a multifocal IOL, as are patients who do not benefit from the summation of binocular multifocality (monofocalists)(32)patients with irregular astigmatism, corneal and pupillary abnormalities(33). Astigmatism should always be corrected, so a topography is required before surgery in order to choose a multifocal toric IOL.
Diffractive IOLs
Diffractive IOLs have rings on the surface resulting in a discontinuous optical density(34). Apodised diffractive IOLs are characterised by a gradual reduction in the height of diffractive steps from the centre to the periphery (33,34). Non-apodised IOLs have uniform step heights from the centre to the periphery, so that light is equally distributed in both focal points regardless of pupil size (33,34).
These are diffractive IOLs: AT Lisa tri 389 MP (Carl Zeiss Meditec, Henningsdorf, Germany), FineVision (PhysIOL SA, Liège, Belgium), Acrysof IQ Pan 0ptix (Alcon Lab, Fort Worth, Texas, USA).
Refractive IOLs
Refractive IOLs have concentric zones with different dioptric powers to achieve multifocality.
Rotational symmetry IOLs (ReZoom, Abbot Medical Optics (AMO), Irvine, California, USA) allow good distance and intermediate vision, but limited near vision. Other limitations include pupil dependence, halos, glare and high sensitivity to lens centration.(33)
Rotational asymmetry IOLs are a newer version of refractive IOLs; they have a lower segment with an additive for near and an aspheric zone for distance vision with a smooth transition between the two zones. They provide good near, intermediate and distance vision with minimal dysphotopsia as light hitting the transition zone is reflected off the optical axis preventing diffraction.(35)
These IOLs include: Lentis Mplus (Oculentis GmbH, Berlin, Germany), and SBL-3 IOL (Lenstec. Inc., Christ Church, Barbados)
Extended Depth of Focus IOLs - EDOF
Extended Depth of Focus (EDOF) IOLs instead of creating several focuses like multifocal IOLs create a single elongated focal point in order to increase the depth of focus, reducing dysphotopsias.(36) Although intermediate distance vision is excellent with EDOF IOLs, there is a reduction in the quality of near vision (37,38) due to induced aberrations.(36)
Pure EDOF IOLs are based on the pinhole effect, such as the IOL IC-8 (AcuFocus Inc, CA, USA), or on spherical aberration such as the IOL Mini WELL Ready (SIFI, Catania, Italy).(36)
Hybrid multifocal EDOF IOLs utilise chromatic aberrations, diffractive/refractive EDOF optics, or additional power to enhance near vision.(36) The Tecnis Symfony ZXR00 (Johnson and Johnson Vision, Jacksonville, FL) and the At Lara 29 MP (Carl Zeiss Meditec, Jena, Germany) are examples of EDOF/refractive IOLs, the Lucidis (Swiss Advanced Vision, SAV-IOL SA, Neucha?tel, Switzerland) is an EDOF/refractive IOL, and the InFo - Instant Focus IOL (Swiss Advanced Vision, SAV-IOL SA, Neucha?tel, Switzerland) is an EDOF refractive-diffractive IOL.
Clinical and visual results
Patient satisfaction and visual function with multifocal IOLs are generally very good(39). Multifocal IOLs bring uncorrected distance and near visual acuity to high levels. Trifocal IOLs achieve better objective and subjective results than bifocal IOLs (45). Results in terms of distance and near visual acuity are generally better with diffractive multifocal IOLs than with refractive multifocal IOLs (33).
An effective way to compare premium IOLs is through the defocus curve, as it allows comparison of distance, intermediate distance and near vision achieved with each IOL (Fig. 4).
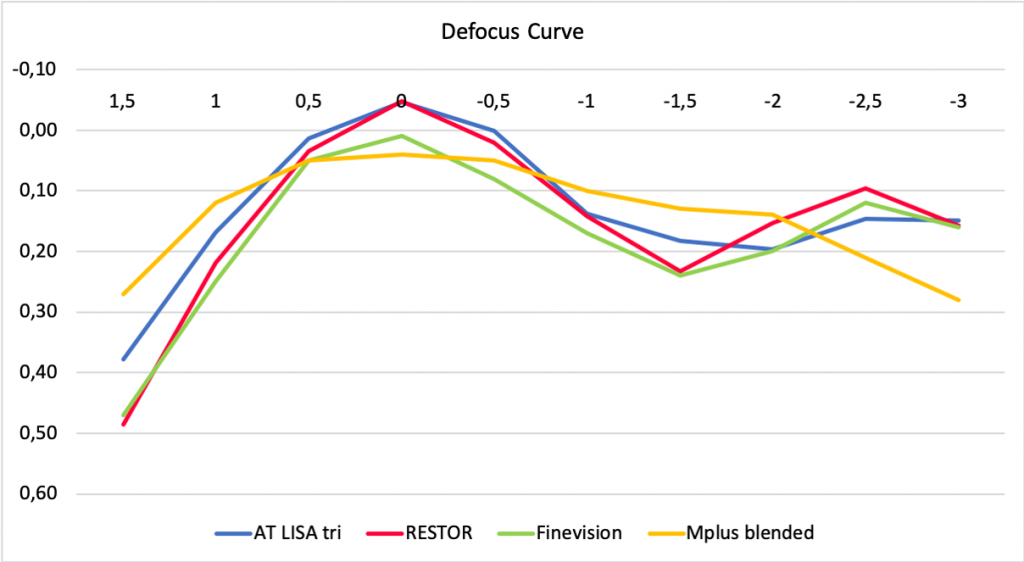
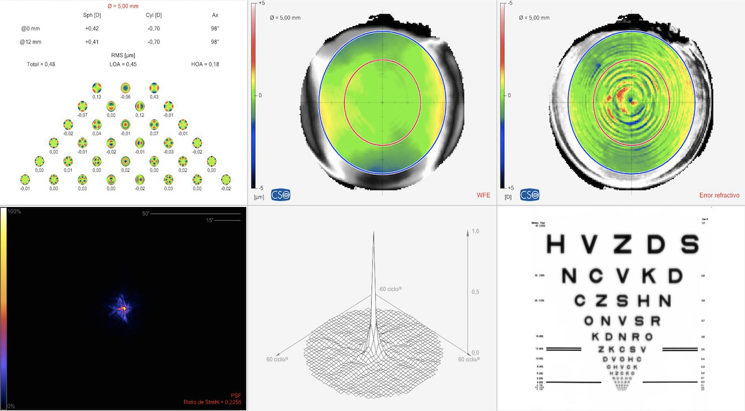
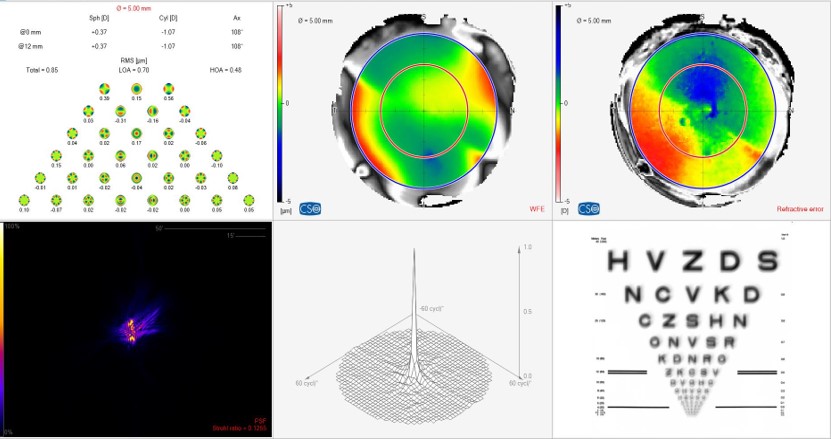
Higher-order aberrations play an essential role in determining retinal image quality, and can be induced by IOLs and influenced by pupil size (Figs. 5-6).
Compared with monofocal IOLs, multifocal IOLs typically result in more intraocular aberrations (46)although the results in terms of contrast sensitivity are comparable for monofocals and multifocals47).
Causes of patient dissatisfaction
The main cause of dissatisfaction is blurred vision, which can be secondary to a wide pupil, residual ametropia and astigmatism, posterior capsule opacification and dry eye(33). The second cause of dissatisfaction is the presence of dysphotopsia, such as halos and glare, which occur more frequently after implantation of a refractive IOL (33).
The most frequent causes of multifocal IOL explantation and lens replacement are decreased contrast sensitivity, dysphotopsia, failure in the neurofitting process, incorrect IOL power, excessive preoperative expectations, IOL decentration and anisometropia (33).
Neuroadaptation
Neuroadaptation is a process in which the brain learns how to 'correct' the image in order to use it appropriately so that the final perception is as real as possible. This process is easier in younger patients. It takes a minimum of three months for the dysphotopsias to diminish significantly, and reaches its peak one year after surgery. A failure in the neuroadaptation process can cause distortion, confusion, a feeling of poor vision and the perception of glare.(33). All patients implanted with a multifocal IOL go through a process of neuroadaptation.
Our group pioneered the treatment of neuroadaptation failure by changing the optics of multifocal IOLs (e.g. a multifocal refractive IOL to a multifocal diffractive IOL) with good results.
Future perspectives in realising multifocality
The development of increasingly advanced technology for measuring and understanding aberrations and their effects on vision quality has led to great advances in the development of intraocular implants. Hybrid multifocal EDOF IOLs are a promising technology that will aid the process of post-implant neuroadaptation. Now the focus shifts to the possibility of restoring the individual's power of accommodation, either by filling the capsular bag with polymers that mimic the natural crystalline lens(48)more specifically with the creation of intraocular implants with ever-increasing accommodative capacities (49).
Conclusions
At present, most of the techniques available to achieve multifocality are adequate and effective. Treatment is individualised to meet the patient's needs and maximise vision at all distances. The need in the pre-operative planning phase for careful screening and patient selection and a full disclosure of the risks and benefits associated with each treatment option cannot be overemphasised.
Authors: Veronica Vargas, MD1,2; Joan Balgos, MD1,2; Jorge Alió, MD, PhD, FEBO1,2,3
1 Cornea, Cataract and Refractive Surgery Department, VISSUM Alicante, Spain.
2 Research & Development Department, VISSUM Alicante, Spain.
3 Universidad Miguel Hernández, School of Medicine, Alicante, Spain.
Financial Support
This article was partly supported by Red Temática de Investigación Cooperativa en Salud (RETICS), reference number RD16/0008/0012, funded by Instituto Carlos III - General Subdirection of Networks and Cooperative Investigation Centres (R&D&I National Plan 2008-2011) and the European Regional Development Fund (Fondo Europeo de Desarrollo Regional FEDER)
For correspondence:
Prof. Jorge L. Alió, MD PhD, FEBO
Calle Cabañal, 1 - Edificio Vissum. 03016, Alicante, Spain
E-mail: jlalio@vissum.com
Ph.: 0034 672 398 765
Bibliographic references
1. Vargas V, Radner W, Allan B, Reinstein D, Burckhard D, Alió JL. Methods for the study of near, intermediate vision and accommodation: An overview of subjective and objective approaches. Survey of Ophthalmology (2018), doi: 10.1016/j.survophthal.2018.08.003.
2. Alió JL, Alió del Barrio JL, Vega-Estrada A. Accommodative intraocular lenses: where are we and where we are going. Eye and Vision 2017;4:16.
3. Holden, B.A., Fricke, T.R., Ho, S.M., Wong, R., Schlenther, G., Cronje, S., Burnett, A., Papas, E., Naidoo, K.S., Frick, K.D., 2008. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol 126, 1731-1739.
4. Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, Naduvilath T, Naidoo KS. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia. Systematic review, meta-analysis and modelling. Ophthalmology 2018, doi.org/10.1016/j.ophtha.2018.04.013
5. Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology 2015;122:1706-1710.
6. Goldberg DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg. 2001;27:1449-55.
7. Reinstein DZ, Couch DG, Archer TJ. LASIK for hyperopic astigmatism and presbyopia using micro-monovision with the Carl Zeiss Meditec MEL80 Platform. J Refract Surg.2009;25:37-58.
8. Davidson RS, Dhaliwal D, Hamilton DR, Jackson M, Patterson L, Stonecipher K, et al. Surgical correction of presbyopia. J Cataract Refract Surg. 2016;42:920-30.
9. Ito M, Shimizu K, Iida Y, Amano R. Five-year clinical study of patients with pseudophakic monovision. J Cart Refract Surg [Internet]. 2012;38(8):1440-5.
10. Alió JL, Chaubard JJ, Caliz A, et al. Correction of presbyopia by technovision central multifocal LASIK (presbyLASIK). J Refract Surg 2006; 22: 453-460.
11. Wan Yin GH, McAlinden C, Pieri E et al. Surgical treatment of presbyopia with central presbyopic keratomileusis: One-year results. J Cataract Refract Surg. 2016;42:1415-1423.
12. Uthoff D, Pölzl M, Hepper D, Holland D. A new method of cornea modulation with excimer laser for simultaneous correction of presbyopia and ametropia. Graefe's Arch Clin Exp Ophthalmol. 2012;250(11):1649–61.
13. Luger MH a., Ewering T, Arba-Mosquera S. One-Year Experience in Presbyopia Correction With Biaspheric Multifocal Central Presbyopia Laser In Situ Keratomileusis. Cornea. 2013;32(0):644-52.
14. Baudu P, Penin F, Mosquera SA. Uncorrected Binocular Performance After Biaspheric Ablation Profile for Presbyopic Corneal Treatment Using AMARIS with the PresbyMAX Module. Am J Ophthalmol. 2013;155:636-47.
15. Luger MHA, Mcalinden C, Buckhurst PJ, Wolffsohn JS, Verma S, Mosquera SA. Presbyopic LASIK Using Hybrid Bi-Aspheric Micro-Monovision Ablation Profile for Presbyopic Corneal Treatments. Am J Ophthalmol. 2015;160(3):493-505.
16. Chan T, Kwok P, Jhanji V, Woo V, Ng A. Presbyopic Correction Using Monocular Bi-aspheric Ablation Profile (PresbyMAX) in Hyperopic Eyes: 1-Year Outcomes. J Refract Surg. 2017;33(1):37-43.
17. Vargas V, Alió JL. Corneal compensation of presbyopia: PresbyLASIK, an updated review. Eye Vis 2017; 13:4-11.
18. Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg.2012;28(8):531-539.
19. Reinstein DZ, Archer TJ, Gobbe M. LASIK for Myopic Astigmatism and Presbyopia using Non-linear Aspheric Micro-monovision with the Carl Zeiss Meditec MEL 80 Platform. J Refract Surg. 2011;27 (1): 23-37.
20. Reinstein DZ, Couch DG, Archer TJ. LASIK for Hyperopic astigmatism and Presbyopia Using Micro-monovision with the Carl Zeiss Meditec MEL80 Platform. J Refract Surg.2009;25:37-58).
21 . Arba Mosquera S, Alió JL. Presbyopic correction on the cornea. Eye and Vision. 2014:1-10.
22. Konstantopoulos A, Metha J. Surgical compensation of presbyopia with corneal inlays. Expert Rev. Med. Devices 2015. 12(3), 341-352.
23. Garza EB, Gomez S, Chayet A, Dishler J. One-Year Safety and Efficacy Results of a Hydrogel Inlay to Improve Near Vision in Patients With Emmetropic Presbyopia. J Refract Surg. 2013;29(3):166-72
24. Whitman J, Dougherty PJ, Parkhurst GD, et al. Treatment of presbyopia in emmetropes using a shape-changing corneal inlay. One-year clinical outcomes. Ophthalmology 2016;123:466-475.
25. Lindstrom RL, Macrae SM, Pepose JS, Hoopes PC. Corneal inlays for presbyopia correction. Curr Opin Ophthalmol. 2013;24:281-7.
26. Tomita M, Kanamori T, Waring G, et al. Simultaneous corneal inlay implantation and laser in situ keratomileusis for presbyopia in patients with hyperopia, myopia, or emmetropia: six-month results. J Cataract Refract Surg. 2012;38:495-506.
27. Tomita M, Kanamori T, Waring G, Nakamura T, Yukawa S. Small- aperture corneal inlay implantation to treat presbyopia after laser in situ keratomileusis. J Cataract Refract Surg. 2013;39:898-905.
28. Alió JL, Abbouda A, Huseynli S, Knorz MC, Emilia M, Homs M, et al. Removability of a Small Aperture Intracorneal Inlay for Presbyopia Correction. J Refract Surg. 2013;29(8):550-6.
29. Shing Ong H, Chan AS, Yau CW, Mehta JS. Corneal inlays for presbyopia explanted due to corneal haze. J Refract Surg.2018;34(5):357-360.
30. Dexl AK, Seyeddain O, Riha W, et al. Reading performance and patient satisfaction after corneal inlay implantation for presbyopia correction: two-year follow-up. J Cataract Refract Surg. 2012;38:1808-1816.
31. Akella SS. Juthani VV. Extended depth of focus intraocular lenses for presbyopia. Curr Opin Ophthalmol 2018; 29:318-322.
32. Braga-Mele R, Chang D, Dewey S, et al. Multifocal intraocular lenses: Relative indications and contraindications for implantation.
33. Alió JL, Plaza-Puche AB, Fernandez-Buenaga R, Pikkel J, Maldonado M. Multifocal Intraocular Lenses: An Overview. Survey of Ophthalmology (2017), doi: 10.1016/ j.survophthal.2017.03.005.
34. Gooi P, Ahmed I. Review of Presbyopic IOLs: Multifocal and Accommodating IOLs. Int Ophthalmol Clin. 2012;52(2):41-50.
35. Moore JE, Mc Neely RN, Pazo EE et al. Rotationally asymmetric multifocal intraocular lenses: preoperative considerations and postoperative outcomes. Curr Opin Ophthalmol 2017, 28:9-15.
36. Kanclerz P, Toto F, Grzybowski A, Alió JL. Extended depth of field intraocular lenses: an update.
37. Alio JL. Presbyopic Lenses: Evidence, Masquerade News, and Fake News. Asia Pac J Ophthalmol (Phila). 2019;8(4):273-274.
38. Böhm M, Petermann K, Hemkeppler E, Kohnen T. Defocus curves of 4 presbyopia-correcting IOL designs: diffractive panfocal, diffractive trifocal, segmental refractive, and extended-depth-of-focus. J Cataract Refract Surg. 2019;45(11):1625-1636.
39. Rosen E, Alió JL, Dick H, Dell S, Slade S. Efficacy and safety of multi-focal intraocular lenses following cataract and refractive lens ex-change : meta-analysis of peer-reviewed publications. J Cataract Refract Surg. 2016;42:310-28.
40. Alió JL, Pikkel J. Multifocal Intraocular Lenses. The Art and Practice. 2nd edition. Springer; 2019.378p.
41. Alió JL, Montalbán R, Peña-García P. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013 Nov; 29(11):756-61
42. Venter JA, Pelouskova M, Collins BM, et al. Visual outcomes and patient satisfaction in 9366 eyes using a refractive segmented multifocal intraocular lens. J Cataract Refract Surg 2013; 39:1477-1484.
43. Savini G, Balducc N, Carbonara C, et al Functional assessment of a new extended depth of focus intraocular lens. Eye.2019 Mar;33(3):404-410
44. Schallhorn SC, Teenan D, Venter JA, et al. Initial Clinical Outcomes of a New Extended depth of focus intraocular lens. J Refract Surg. 2019;35(7): 426-433.
45. Vargas V, Alió JL, Ferreira R, et al. Long-term objective and subjective outcomes following bilateral implantation of diffractive bifocal or trifocal intraocular lenses. Peer reviewed paper.
46. Ortiz D, Alió J, Bernabe?u G, Pongo V. Optical performance of monofocal and multifocal intraocular lenses in the human eye. J Cataract Refract Surg. 2008;34:755-762.
47. Cochener B, Lafuma A, Khoshnood B, Courouve L, Berdeaux G. Comparison of outcomes with multifocal intraocular lenses: a meta-analysis. Clin Ophthalmol. 2011;5:45-56.
48. Kook D, Kampik A, Dexl A, et al. Advances in lens implant technology. F1000 Med Rep. 2013;5(3). doi:10.3410/M5-3
49. Alió JL, Simonov A, Plaza-Puche A, et al. Visual outcomes and ac- commodative response of the Lumina accommodative intraocular lens. Am J Ophthalmol. 2016;164:37-48.
Dr. Carmelo Chines
Direttore responsabile
