Noel Alpins has, in fact, devised new methods for analysing and treating astigmatism and developed ASSORT® software for programming and analysing surgical results, a program widely used by ophthalmologists both in Australia and on other continents.
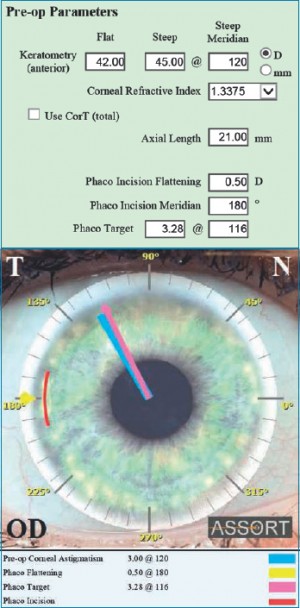
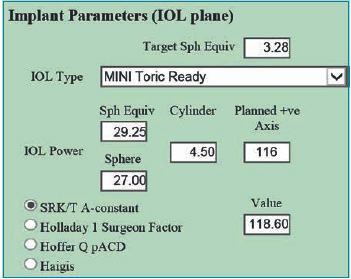
[caption id="attachment_2945" align="alignleft" width="351"]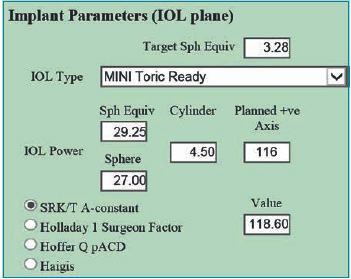 Fig. 2. The spherical and toric parameters of SIFI's Mini Toric Ready IOL[/caption].
Fig. 2. The spherical and toric parameters of SIFI's Mini Toric Ready IOL[/caption].
Why is the position of the incision so important when calculating the power of toric IOLs?The position of the phaco incision for toric IOLs is of paramount importance.
Whatever effect it has on pre-operative corneal astigmatism must be taken into account in the IOL selection process, as well as in its placement.
The surgeon must calculate the effect of the incision on the preoperative corneal astigmatism - with regard to changes in magnitude and/or changes on the meridian.
The selection of IOL toricity will, therefore, be more accurate.
It is important to note that placing the phaco incision on the most curved meridian of the pre-operative astigmatism will have the greatest flattening effect.
Placing the incision in a location other than the most curved meridian will cause an inferior effect along with the rotation of the pre-operative corneal astigmatism.
As one gets closer to 90° from the most curved meridian, astigmatism increases and less rotation occurs.
Why is it better to refer to the Flattening Effect of the primary incision instead of the overall SIA (Surgically induced astigmatism) vector for the calculation of IOL power?
The SIA is composed of theFlattening Effect and the Torsion (Torque).
L'Flattening effect is a measure of how much the magnitude of the pre-operative corneal astigmatism has changed, while the Torsion is the component involved in the rotation of astigmatism from the pre-operative meridian to the post-operative meridian, but not in its reduction.
Using the entire SIA overestimates the effect of the incision in reducing astigmatism and leads to an inaccurate calculation of the corneal astigmatism or its location; as a result, there will be an inappropriate calculation of the IOL toricity required to neutralise the corneal astigmatism.
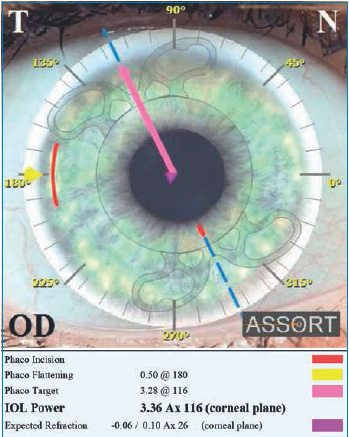
[caption id="attachment_2946" align="alignright" width="349"]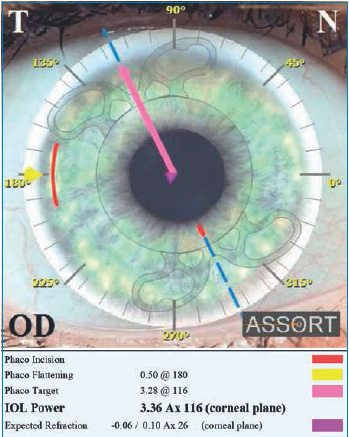 Fig. 3. The SIFI ASSORT Toric IOL Calculator indicates the power of the IOL in the corneal plane and the expected refraction.[/caption]
Fig. 3. The SIFI ASSORT Toric IOL Calculator indicates the power of the IOL in the corneal plane and the expected refraction.[/caption]
Do you think that the latest technological innovations can really improve the management of 'refractive surprise' in post-operative refractive cataract surgery for the correction of astigmatism?
There are basically three options for managing refractive surprise after toric IOL surgery:
1. Rotation of the implanted toric IOL
Using the Toric IOL Assort calculator (www.assort.com), the minimum value of the refractive cylinder that can be achieved by rotating the toric IOL is calculated. If this reduces the refractive cylinder surprise significantly below 1.0 D, then it is only a matter of rotating the implanted toric IOL towards the calculated axis. Ideally, this should be done 4-6 weeks after cataract surgery.
2. Replacement of the implanted toric IOL
Again, using the Assort calculator for toric IOLs, the analysis with the Alpins Method shows the Error Magnitude (ME) which is the difference in magnitude between the Target Induced Astigmatism (TIA) vector and the Surgically Induced Astigmatism (SIA) vector and allows us to know whether the implanted toric IOL is too strong or too weak for astigmatism correction.
If this parameter is significant (0.75 D or higher), then replacement of the toric IOL with a toric corrected lens or the use of a supplementary lens in the ciliary sulcus is recommended.
3. Excimer laser surgery
If the rotation of the implanted toric IOL does not significantly reduce the surprise of the refractive cylinder and the ME is less than +/- 0.75 D, then laser refractive surgery is recommended to correct the residual astigmatism that is probably the result of a multiple set of causes.
Finally, are there major differences in the treatment approach to astigmatism in Europe and Australia?
The approach to astigmatism is very similar in Europe and Australia - in both contexts we have the advantage of having the most advanced technology available, including the latest in IOL design, surgical and diagnostic equipment.
My personal approach to surgical correction of astigmatism depends on the extent of the astigmatism to be corrected:
- - 0,50 - 0,75 D a single 2.2 mm incision in a clear cornea
- - 1,00 - 2,00 D a single clear corneal axis incision (3.0 mm) + a single LRI (180° from the clear corneal incision).
- - > 2.00 D Toric IOL with 2.2 mm phaco incision
If there are no signs of lenticular opacities and the patient is suitable for laser refractive surgery I use vector planning for optimal treatment of astigmatism.
In many cases where there is residual ocular astigmatism (ORA - Ocular Residual Astigmatism) due to corneo-refractive differences, vector planning reduces the amount of residual corneal astigmatism post-operatively compared to treatment based on refractive parameters alone, without increasing the residual refractive cylinder post-operatively. Vector planning incorporates both refractive cylinder and corneal astigmatism into the treatment plan, using an optimised approach that takes into account both corneal parameters and refractive cylinder.
Read theinterview in English.
Dr. Carmelo Chines
Direttore responsabile