Ocular pemphigoid is a rare and complex autoimmune disease that primarily affects the conjunctiva, causing chronic bilateral conjunctivitis with progressive scarring. This disorder is part of the larger group of mucous membrane pemphigoids and can lead to serious consequences for vision if not treated properly.
Autoimmune mechanisms
Ocular pemphigoid is a complex autoimmune disease, mainly caused by a type II autoimmune response, in which the body mistakenly attacks its own tissue. Antibodies bind to antigens on the basement membrane of the conjunctiva, triggering an inflammatory reaction.
This process activates complement proteins and inflammatory cytokines. The result is chronic inflammation that leads to scarring of the conjunctiva.
It is important to note that, despite the involvement of autoantibodies, these are not always easily detectable in patients. Therefore, diagnosis is often based on a combination of clinical symptoms and histopathological tests.
Genetic and Environmental Factors
In addition to autoimmune mechanisms, the genetic factors play a significant role: it has been observed that individuals with specific HLA types, such as HLA-DR4 and HLA-DQ7, show a higher predisposition to the disease.
However, exposure to environmental factors, such as infections or chemicals, can act as a trigger for the clinical manifestation of the disease.
In summary, a combination of genetic predisposition and environmental factors contributes to the development of ocular pemphigoid, making a personalised approach to diagnosis and treatment essential.
Symptoms and Clinical Signs of Pemphigoid
The symptoms are varied and may evolve over time.
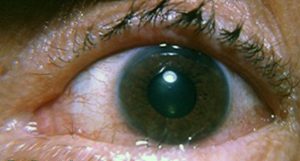
Chronic conjunctivitis is one of the hallmarks of ocular pemphigoid. Patients often complain of eye redness, lacrimation and a foreign body sensation. These symptoms can easily be mistaken for other eye conditions.
As the disease progresses, symptoms become more prominent and persistent. Chronicity of symptoms is accompanied by periods of remission and flare-ups, characteristic of many autoimmune diseases.
Disease Progression
The progression of ocular pemphigoid can lead to serious complications such as conjunctival scarring and corneal opacification. Initially, mild inflammation is observed, but with time, it may develop simblefaron and other ocular adhesions.
Scarring progresses, causing more severe symptoms and complications such as entropion or trichiasis. Without proper treatment, the condition can lead to significant vision loss.
Early recognition of progressive symptoms is crucial to prevent long-term adverse outcomes.
Pemphigoid Diagnosis
Early diagnosis is essential to avoid complications. Diagnostic tools vary from histopathological methods to clinical evaluation systems.
Histopathological methods
 The conjunctival biopsy with direct immunofluorescence is the standard method of diagnosis. This test detects the linear deposition of IgG, IgA and sometimes IgM in the epithelial basement membrane area.
The conjunctival biopsy with direct immunofluorescence is the standard method of diagnosis. This test detects the linear deposition of IgG, IgA and sometimes IgM in the epithelial basement membrane area.
However, approximately 20% - 40% of patients may have negative biopsy results despite clinical symptoms. This does not exclude the diagnosis, but emphasises the importance of correlating histopathological findings with clinical symptoms.
Histological analysis, including stains such as H&E, PAS and Giemsa, offers further details on the inflammatory state and can differentiate the disease from other conditions.
Evaluation Systems
Various evaluation systems help in monitoring the progression of ocular pemphigoid. The Foster's system and that of Mondino and Brown are commonly used to classify the severity of the disease.
Foster's system is based on clinical signs, while Mondino and Brown's system assesses the depth of the lower fornix. These classifications guide therapeutic decisions and help monitor the evolution of the disease.
Treatment of pemphigoid
Treatment focuses on managing inflammation and preventing scarring. Treatment options include topical and systemic therapies adapted to the individual needs of patients.
Le topical therapies are essential to relieve symptoms and improve ocular comfort. The use of preservative-free artificial tears and lubricating ointments is recommended to maintain the moisture of the ocular surface.
I topical corticosteroidscyclosporin-A and tacrolimus can reduce ocular inflammation, but must be used with caution to avoid side effects. In severe cases, autologous serum drops can promote epithelial healing.
Finally, the use of scleral lenses can provide physical protection and hydration to the ocular surface, although they require regular monitoring to avoid complications.
I systemic treatments are crucial in halting the progression of the disease. Dapsone is the first-line treatment for mild or moderate cases, while immunosuppressants such as azathioprine or methotrexate are used in more severe forms.
In advanced cases, systemic corticosteroids or biological therapies such as rituximab may be required. These options aim to reduce autoimmune activity and systemic inflammation.
Multidisciplinary Management
 The effective management of Ocular Pemphigoid requires a multidisciplinary approach, involving various specialists to optimise treatment and follow-up.
The effective management of Ocular Pemphigoid requires a multidisciplinary approach, involving various specialists to optimise treatment and follow-up.
A interprofessional team of ophthalmologists, dermatologists, rheumatologists and other specialists must work together to provide integrated and customised treatment.
- Coordinate care to ensure optimal treatment.
- Monitor the response to treatment and adapt therapies.
- Identifying and managing complications in a timely manner.
This collaboration reduces the risk of disease progression and improves the patient's quality of life.
The regular follow-up is essential to monitor disease progression and modify treatment as necessary. Prognosis varies depending on the severity of the disease and response to treatment.
- Systemic therapy halts progression in about 90% of patients.
- The recidivism rate is 20% - 30%.
- Effective management reduces the risk of blindness and other complications.
On the subject of eye inflammation see also:
- Ocular syphilis: increasing incidence globally - Oculista Italiano
- Microbiota and ocular inflammation - Oculist Italiano
- Hingorani M, Lightman S. Ocular cicatricial pemphigoid. Curr Opin Allergy Clin Immunol. 2006 Oct;6(5):373-8
- Ocular Pemphigoid - StatPearls - NCBI Bookshelf
